- Research article
- Open access
- Published: 24 February 2020

A quasi-experiment assessing the six-months effects of a nurse care coordination program on patient care experiences and clinician teamwork in community health centers
- Ingrid M. Nembhard ORCID: orcid.org/0000-0001-7696-4832 1 ,
- Eugenia Buta 2 ,
- Yuna S. H. Lee 3 ,
- Daren Anderson 4 ,
- Ianita Zlateva 4 &
- Paul D. Cleary 5
BMC Health Services Research volume 20 , Article number: 137 ( 2020 ) Cite this article
16k Accesses
10 Citations
6 Altmetric
Metrics details
Recognition that coordination among healthcare providers is associated with better quality of care and lower costs has increased interest in interventions designed to improve care coordination. One intervention is to add care coordination to nurses’ role in a formal way. Little is known about effects of this approach, which tends to be pursued by small organizations and those in lower-resource settings. We assessed effects of this approach on care experiences of high-risk patients (those most in need of care coordination) and clinician teamwork during the first 6 months of use.
We conducted a quasi-experimental study using a clustered, controlled pre-post design. Changes in staff and patient experiences at six community health center practice locations that introduced the added-role approach for high-risk patients were compared to changes in six locations without the program in the same health system. In the pre-period (6 months before intervention training) and post-period (about 6 months after intervention launch, following 3 months of training), we surveyed clinical staff ( N = 171) and program-qualifying patients (3007 pre-period; 2101 post-period, including 113 who were enrolled during the program’s first 6 months). Difference-in-differences models examined study outcomes: patient reports about care experiences and clinician-reported teamwork. We assessed frequency of patient office visits to validate access and implementation, and contextual factors (training, resources, and compatibility with other work) that might explain results.
Patient care experiences across all high-risk patients did not improve significantly ( p > 0.05). They improved somewhat for program enrollees, 5% above baseline reports ( p = 0.07). Staff-perceived teamwork did not change significantly ( p = 0.12). Office visits increased significantly for enrolled patients ( p < 0.001), affirming program implementation (greater accessing of care). Contextual factors were not reported as problematic, except that 41% of nurses reported incompatibility between care coordination and other job demands. Over 75% of nurses reported adequate training and resources.
Conclusions
There were some positive effects of adding care coordination to nurses’ role within 6 months of implementation, suggesting value in this improvement strategy. Addressing compatibility between coordination and other job demands is important when implementing this approach to coordination.
Peer Review reports
Efforts to improve care coordination have increased in recent years due to the recognition that coordination is a central part of high quality care yet is often less than optimal in healthcare [ 1 , 2 , 3 , 4 ]. Care coordination refers to “the deliberate organization of patient care activities between two or more participants (including the patient) involved in a patient’s care to facilitate the appropriate delivery of healthcare services” ([ 5 ], p., 5]). In the United States (U.S.), 35% of patients with serious illnesses or chronic conditions report having experienced a coordination failure [ 6 ]. Such failures have resulted in medical complications, preventable hospitalizations, duplicative testing, and morbidity increases [ 4 ] estimated to cost the U.S. healthcare system $25 to 45 billion in 2011 [ 7 , 8 ]. Other countries (e.g. Canada, France, Norway, Sweden, and Switzerland) struggle with care coordination as well, where 30% or more of patients report experiencing coordination failures [ 6 ].
To improve care coordination in several countries [ 4 , 9 , 10 , 11 ], many health systems and organizations have implemented or are implementing nurse care coordination initiatives in which nurses provide additional care and support to patients with coordination needs such as those with a chronic illness, transitioning from hospital to home, or with multiple medical and behavioral health issues [ 12 , 13 , 14 ]. In this approach, nurses work closely with designated patients and providers to coordinate multi-specialty care and help patients manage their illnesses. Core responsibilities in this role include monitoring patient health and facilitating development, communication, and delivery of care plans with other care team members [ 15 , 16 ]. Nurses in many organizations perform these activities, which are within their scope of practice [ 17 , 18 ]. New programs have structured these activities, clarifying authority, tasks, options, and responsibility, to enhance nurses’ visibility, effectiveness, and efficiency as coordinators. These programs address calls from professional and scientific groups for nurse coordinator roles to be more explicit, developed, and designed deliberately into training and delivery organizations [ 15 , 18 , 19 , 20 ]. These programs should lead to better experiences for patients and clinicians because assignment of responsibility to one person and coordination improve the logic, continuity, and efficiency of care [ 5 , 12 , 18 , 21 , 22 , 23 ].
Currently, two approaches to nurse care coordination are common. In the first, adopted mainly in large health systems and medical groups, a nurse serves exclusively as care coordinator for a panel of patients. This “exclusive-role approach,” has been used, for example, by participants in the U.S. Medicare Care Coordination Demonstration program [ 24 ]. In the second “added-role approach”, a nurse performs care coordination in addition to existing responsibilities. Although reviews of research on the first approach indicate mixed results [ 25 , 26 , 27 ], increasing evidence from controlled trials indicates that patients with these coordinators experience better technical quality of care, lower hospital readmissions, lower costs, and better care experiences (e.g., provider-patient communication) than patients who do not have a coordinator [ 12 , 17 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 ].
Little is known about the experiences of patients served by nurses in the added-role approach, which may be pursued more by smaller organizations or those in lower-resource settings, which are many of the settings across the world. There is also limited information, particularly in primary care settings about the effectiveness of this approach, even though these settings are increasingly expected to coordinate care with patients and other providers [ 38 ]. In primary care settings such as federally qualified health centers (FQHCs) in the U.S., a type of community health center that serves disproportionately more complex patients with multiple co-morbidities and socioeconomic disadvantages than do private practices and health systems [ 39 ], the imperative for coordination is especially great, but there is little evidence about the effects of adding care coordination to the nursing role. Nurses dedicating any increased attention to these tasks may be positive for patients in need and clinicians. On the other hand, the potential positive effects of the added-role approach may not be realized because of the inability to focus exclusively on coordination tasks.
In this manuscript, we examine the early (six-month) effects of a nurse care coordination program in FQHC practices that use the added-role approach for high-risk patients using two measures: care experiences of these patients and clinician-reported teamwork. High-risk patients have complex and/or multiple medical and psychosocial problems, which may require them to see as many as 16 physicians per year, making them most in need of care coordination, most at risk for coordination failures, and most likely to benefit from care coordination, [ 1 , 40 ] although recent studies suggest that benefits may extend beyond this group [ 41 ]. We also examine an indicator of implementation effectiveness, the frequency of patient office visits, and contextual factors because they can influence implementation, and thus program outcomes [ 42 ].
We focus on effects in the program’s first 6 months because early experiences with a program are often consequential for long-term success [ 43 , 44 , 45 , 46 ]. Also, departure from past patterns is often salient to participants early, before they become accustomed to new patterns and adjust expectations, [ 47 ] making early assessments a window into program functioning. Currently, there is limited investigation of the early effects of nurse care coordination programs, leaving organizations with little knowledge about what to expect. Research on other patient-nurse and coordination interventions in other settings (e.g., skilled nursing visits in home health care [ 48 , 49 , 50 ]) suggests that positive effects can materialize in 6 months.
Study setting and design
This study was conducted in a statewide, multi-site FQHC with 12 sites that provide comprehensive primary medical, dental, and behavioral healthcare services to over 140,000 patients a year. The center serves patients with all types of primary care needs and emphasizes serving the uninsured, underinsured, and special populations such as patients with HIV/AIDS, diabetes, and chronic mental health issues. The FQHC has been recognized as a Primary Care Medical Home by the Joint Commission [ 51 ] and a level 3 Patient-Centered Medical Home by the National Commission on Quality Assurance [ 52 ]. Thus, each site has demonstrated commitment to patient-centered care, comprehensive care, coordinated care, access to care, and a systems-based approach to quality and safety.
We conducted a cluster quasi-experiment in which pre-post intervention changes in clinician and patient experiences in six sites (clusters) that introduced a nurse care coordination program for high-risk patients using the added-role approach (“intervention group”) were compared to changes in experiences in six sites without the program at the time of our study (“comparison group”). Sites in the comparison group implemented the program after our data collection. The FQHC used a sequential roll-out plan (all locations (3) in one county every 3 months) as it does for certain large-scale initiatives for operational reasons (e.g., maintaining cross-coverage between providers in county and having sufficient resources for implementation). When deciding about comparison sites, the FQHC's leadership selected pairs of sites that were relatively similar based on number of patients, patient population profile, and the organization of sites. Sites were allocated to the intervention group if the intervention could begin sooner there than at pair site, given staff work and training schedules, etc. The selected intervention and comparison sites were similar at baseline and follow-up on all but two characteristics for which we could obtain data (Table 1 ). Wilcoxon rank-sum tests indicated that the groups differed significantly with respect to percent of patients with Medicare as their health insurer ( p = 0.02 and p = 0.01 at baseline and follow-up, respectively) and percent of patients with “other race” ( p = 0.05 at baseline). We adjust for these differences in our analyses.
Our primary study outcomes were two indicators of program effectiveness: patient reports about their care experiences and clinician reports of teamwork in their centers. If care coordination programs function as intended, patient experiences, as reflected in responses to questions about care coordination, timeliness of care, and support for self-management should improve, as should clinician teamwork.
Because degree and fidelity of program implementation are critical determinants of program effectiveness, we collected the implementation information that we could, given resource limitations and concerns about staff burden. We obtained information about numbers of telephone calls to patients, but those data turned out to be inconsistent and of poor quality and so are not presented. The other measure of program implementation that we have is the number of patient office visits, which is a proxy measure of accessibility of care, engagement with patients, monitoring, and follow-up to achieve care plan goals (e.g., condition controlled, no preventable hospitalization). If the care coordination program was implemented as intended, there should be an increase in patient office visits in the early months of the program to address outstanding patients’ care needs and self-management training. Research on programs that incorporate the exclusive-role approach has found that primary care office visits increase with coordination programs in the first 2 years, while emergency department visits decline for high utilizers [ 53 ]. Over a longer period, not covered by this study, office visits should decline due to better patient health and self-management. Because implementation and effectiveness are often influenced by resources, training, and compatibility with current work, [ 42 , 54 , 55 ] we also assessed these contextual factors via nurse surveys, because these factors may help explain our results. Other non-program specific contextual factors (e.g., employee workload, patient population profile, and supervisor support for workers, which shapes work climate) were examined as well (Table 1 ).
Intervention
In intervention sites, every nurse’s role was expanded to include care coordination for adult patients who were expected to benefit most from this effort. These were defined by the organization as patients who were 18 years of age or older, had two or more visits with a primary care provider (PCP) in the past 12 months, and had been identified as “high risk.” Patients were classified as high risk if they had: 1) two or more emergency room visits in the past 12 months; 2) one or more hospitalizations in the past 12 months; 3) a Type 2 diabetes diagnosis on their problem list and a hemoglobin A1C test in the past 12 months greater than 9%; 4) a diagnosis of persistent asthma diagnosis on problem list and two or more asthma control test scores < 19 in the past 12 months; or 5) four or more of specified chronic illnesses on their active problem list, including Type 2 diabetes, chronic obstructive pulmonary disease, hypertension, asthma, coronary artery disease, or behavioral health diagnosis. A subset of the eligible patients (those with greatest immediate need as perceived by staff) was enrolled in the program at the outset due to time and resource constraints. Other patients were also enrolled when a PCP or nurse identified the patient as needing care coordination (e.g., newly discharged from a hospital).
As part of the new program, nurses were expected to work with enrolled patients to help them navigate their healthcare and lead a weekly panel management meeting with enrollees’ PCP and behavioral health provider. The sessions were to be used to review patient progress, identify additional patients who needed coordination, and plan coordinated care. To implement the program, the organization introduced the nurse care coordinator role to all staff via meetings and other communications (e.g., newsletters). It also provided three resources to nurses to support their effectiveness as coordinators: training, a “playbook”, and an electronic dashboard. All nurses in the intervention sites received 23 h of training over a period of 2 to 3 months from experts within the organization and outside consultants. The training covered care plan development, panel management, documentation, transition care support, motivational interviewing, self-management goal setting, chronic disease management, and behavioral health disorders — evidence-based components of nurse care coordination [ 17 ]. The playbook provided instructions for each task within the new nurse role, information on additional resources, and measures to evaluate performance. The electronic dashboard leveraged information in the organization’s electronic health record system, which aided nurse tracking of patients and activities. No other group was assigned care coordination responsibilities. The organization reinforced its commitment to the role change by monitoring nurse performance and providing feedback reports to nurses. It was expected that the program would lead to more coordinated and timely care, greater patient support for self-management, and care for mental health.
Study outcomes
Patient care experiences.
We collected patient surveys that asked about care experiences during two periods at each center. The first (baseline) period covered the 6 months prior to start of nurse training in the intervention centers, and was before nurses were told about the intervention and patients who would be in the program were known. In intervention and comparison centers, we invited a random sample of the high-risk (i.e., program-eligible) patients described earlier that had visited the center in the preceding 6 months ( N = 5525) to complete the Consumer Assessment of Healthcare Providers and Systems Clinician & Group (CG-CAHPS) survey [ 56 , 57 ] and Patient-Centered Medical Home (PCMH) Supplemental Item Set [ 57 , 58 ]. These surveys assess multiple aspects of patient care experiences, [ 57 , 59 ] and have been used in other studies of care coordination [ 60 , 61 ]. The sites already administered these surveys for performance monitoring. With funding provided by the CAHPS Program, we supplemented sites’ surveying to capture the patients in this study.
We assessed the program’s impact using patients’ responses to questions about four aspects of care targeted by the program and therefore expected to be affected by experiencing the program: timeliness of care, coordination of care, support for patient self-management, and care for mental health. Timeliness of care was hypothesized to increase because patients in the program would have priority access to care; their nurse care coordinators would try to be highly responsive. Coordination of care for program enrollees was to improve because nurses would focus on ensuring that enrollees’ needs were met as seamlessly as possible. Support for self-management and care for mental health were additional program foci and areas of training for nurses; therefore, we expected that nurse efforts in these areas would be reflected in patient reports of their experiences. We focused on these four standard measures of patient care experience, rather than care coordination alone, recognizing that nurse care coordination efforts should manifest in multiple ways [ 19 , 20 ]. Table 2 , Part A lists the items used from the CG-CAHPS survey to measure these aspects of care, response options, and the reliability of the scales in our sample. Patients indicated whether they experienced the action described in each question using a four-point scale (1 = never to 4 = always) or No (=1)/Yes (=4) response. We averaged responses for the items in each composite to arrive at a score for each aspect of their experience. The four composite scores are highly correlated ( p -values < 0.001), so to simplify analyses and presentation, we averaged them to arrive at an overall patient care experience score for each person.
After the program had been in effect for 6 months following nurse training, we again invited a random sample of program-eligible patients that had visited the center in the preceding 6 months ( N = 4661) to complete the CG-CAHPS survey with additional items. All 145 program enrollees received an invitation by design. Follow-up at 6 months allowed us to avoid contamination of the comparison group: per the organization’s fixed roll-out plan, the program (training) was scheduled to begin in the first set of comparison centers at this time. This planned endpoint also aligned with our study objective to assess early effects of the added-role approach.
In both the baseline and follow-up periods, we mailed a copy of the survey in English and Spanish to each patient in the sample. Approximately 2 weeks after the first mailing, members of the sample were sent a thank you/reminder postcard. Approximately 2 weeks after that, another survey package was mailed to those who had not responded. If no response was received after two to three more weeks, we called the patients. A minimum of six calls per person were made on different days and at different times of the week.
In the baseline period, 3209 patients of the 5525 contacted (58%) answered the survey; of those, 3007 (94%) confirmed having visited the center in the prior 6 months (intervention group = 934; comparison group = 2073). In the follow-up period, 2306 patients of the 4661 contacted (49%) answered the survey; of those, 2101 (91%) confirmed having visited the center in the prior 6 months (intervention group sample size = 774; comparison group sample size = 1327). In total, 943 patients answered the survey in both periods (643 in control group; 300 in intervention group), and 113 program enrollees responded (78% of the 145 enrolled).
During the month in which we began both the baseline and follow-up patient surveys, we administered an “organizational assessment survey” via the internet or paper to all primary care team members (PCP, nurses, medical assistants, and behavioral health providers). We recruited team members to participate via informational presentations during lunchtime staff meetings and email, and confirmed willingness to participate via signed consent forms. The survey consisted of validated survey scales for assessing core aspects of teamwork i.e., relational coordination and interprofessional collaboration [ 62 , 63 , 64 ]. Interprofessional collaboration refers to the degree of cooperation among individuals with different disciplinary backgrounds [ 65 ], while relational coordination refers to the presence of high-quality communication and relationships characterized by shared goals, shared knowledge, and mutual respect needed for task integration [ 66 ]. Each scale included four items (Table 2 , Part B). Team members indicated their level of agreement with each item using a four-point response scale (1 = strongly disagree to 4 = strongly agree). Because scores for the two scales were highly correlated ( p < 0.001), we averaged them to arrive at a summary teamwork score reported by each respondent.
At baseline, 96 of 190 (51%) team members completed the survey (intervention group = 43; control group = 53). At follow-up, 135 of 188 (72%) members completed the survey (intervention group = 57; control group = 78). Sixty members participated at both baseline and follow-up. We used their responses in our analyses to assess program effect based on the experiences of a stable population and minimize the possible confounding effect of respondents new to the centers. This longitudinal sample was 39% PCPs, 22% nurses, 24% medical assistants, and 15% behavioral health providers. The majority were female (71%), full-time staff (89%), and with the organization more than 2 years (82%). Except for the percentage with more than 2 years with the organization (63%), this sample was demographically like the full sample consisting of 33% PCPs, 23% nurses, 28% medical assistants, 18% behavioral health providers, 83% female, and 88% full-time staff.
Implementation measures
- Office visit frequency
We obtained information about patients’ number of office visits via response to a question in the CG-CAHPS survey: “In the last 6 months, how many times did you visit this provider to get care for yourself?” Seven response options were offered: none, 1 time (coded as 1), 2 (coded as 2), 3 (coded as 3), 4 (coded as 4), 5 to 9 (coded as 7, the midpoint), and 10 or more times (coded as 10). Patients who did not recall any visits were excluded from study ( N = 202 (7%) at baseline and 205 (9%) at follow-up).
Contextual factors: training, resources, and compatibility with other job demands
The organizational survey administered to primary care team members during the follow-up period included additional questions for nurses about program training, resources, and their new role’s compatibility with other job demands, which we used to assess whether these factors posed a challenge to implementation and effectiveness. Four items were adapted from Venkatesh et al.’s [ 67 ] facilitating attributes scale: “I have the resources necessary to coordinate care for complex patients,” “I have the knowledge necessary to coordinate care for complex patients,” “Coordinating care for complex patients is not compatible with other tasks that I’m required to perform,” and “It is easy for me to coordinate care for complex patients.” A fifth resource-related item drew from the FHQC’s employee survey: “I have adequate authority to carry out my work.” We asked nurses at intervention centers to report their level of agreement with each statement (1 = strongly disagree to 4 = strongly agree). Other non-program specific contextual factors that can affect implementation (e.g., supervisor support for workers and workload) and could be assessed for intervention and comparison groups at baseline and follow-up were evaluated for potential inclusion as covariates.
In models assessing patient care experience (study outcome) and office visit frequency (implementation indicator), we included person-level characteristics that have been shown to be related to reports about healthcare experiences: age, gender, education, race/ethnicity, overall health status, and mental health status [ 68 ]. These were all collected via the CG-CAHPS survey, measured as categorical variables (see Table 3 for categories), and treated as time-varying covariates because some could change from baseline to follow-up. In models assessing teamwork, we included person-level characteristics, obtained via the staff survey, that may influence interactions: profession, gender, full-time status, and years in the organization. In all models, we included characteristics that differed between intervention and comparison centers: percent of patients with Medicare and other race. Characteristics that did not differ were not included.
We conducted two analyses of patient care experience. First, we used a differences-in-differences approach to assess whether the difference in experiences between baseline and follow-up in intervention centers differed significantly from the corresponding difference observed in comparison centers, using data from all survey respondents. This intent-to-treat approach assesses whether the program affected care for all program-qualifying patients at intervention sites, not just enrollees. We used separate mixed linear, also termed multi-level, regression models that included fixed effects for intervention group status (0 = comparison group, 1 = intervention group), period (0 = baseline, 1 = follow-up), intervention-by-period interaction, and covariates. We also included random effects for person, PCP, and center to account for clustering and correlation between repeated measures of the same person, between persons affiliated with the same PCP care team, and between PCP care teams within the same center, respectively. In the models, we focused on the intervention-by-time interaction term, which indicate whether the change over time in the intervention centers was greater than in comparison centers (i.e., whether there was a significant program-intervention effect). Our second set of analyses compared the experiences of only patients enrolled in the coordination program at intervention sites ( N = 95 with complete data of the 113 enrolled) to the experiences of eligible patients at comparison sites. We included the baseline data from all surveyed patients because all were program-eligible. This focused, sub-group analysis assessed the effect of the program on those treated.
For our analysis of teamwork, we again used mixed linear regression models that accounted for clustering within clinics and included fixed effects for intervention group status, period, intervention-by-period interaction, and covariates. We analyzed data from clinicians who had complete data in both the baseline and follow-up surveys as noted above, and again studied difference-in-differences. We used this same statistical technique to assess changes in office visit frequency, our implementation indicator. We present adjusted least squares (LS) means with associated standard errors for our measures.
For our analysis of contextual factors, we calculated the percentage of nurse respondents ( N = 27) who agreed or strongly agreed (response of 3 or 4) with each of the statements in the contextual factors measure. We regarded percentages of 75% or greater as indicative that the factor did not substantially undermine implementation and outcomes.
Table 3 presents participating patients’ characteristics at baseline and follow-up for intervention and comparison centers. Intervention center patients were younger, less educated, and less likely to be White ( p < .05), but did not differ with respect to gender and health status.
Our first analysis of patient care experiences, using data from all survey respondents, indicated that there was not a statistically significant difference in changes between intervention and comparison groups ( p > 0.10). In other words, the program did not change the experience of patients at intervention centers as a whole significantly. Our second analysis focused on program enrollees, however, showed modest improvement in care experiences for this subgroup ( p = 0.07).
Table 4 shows the results of the focused analysis, as well as our analysis of changes in clinician teamwork and patient office visit frequency, our program implementation indicator. The table presents the adjusted LS-means for each measure in intervention and comparison groups at baseline and follow-up and for the difference in change from baseline to follow-up between the two groups (difference-in-difference). Row 1 shows that patient care experience scores increased in the intervention group (2.75 to 2.88, 5%), while scores in the comparison group remained about the same (with slight decrease from 2.82 to 2.80) ( p = 0.07). Row 2 shows that clinician-reported teamwork increased in the intervention group (3.51 to 3.60, 3%) and decreased in the comparison group (3.49 to 3.38, 3%), however, the difference was not significant ( p = 0.12). Row 3 shows that an increase in office visit frequency, our implementation indicator, occurred in the intervention group (for patients enrolled in the program), while a decrease in office visits occurred in the comparison group. Patients enrolled in the program had 1.33 more visits than those in the comparison group, a significant difference ( p < 0.001). Figure 1 graphically presents the results for each measure.
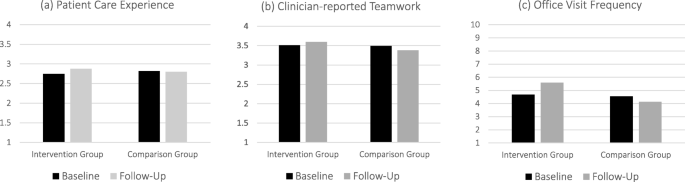
Patient Experience, Clinician-reported Teamwork and Office Visit Frequency for Intervention and Comparison Groups
Most nurse respondents agreed or strongly agreed that training and resources were adequate for their role as care coordinators: 75% (standard error (S.E.) = 0.09) for having the resources necessary; 87% (S.E. = 0.10) for having the knowledge necessary; and 79% (S.E. = 0.10) for having adequate authority to perform the work required – all theorized prerequisites for the coordination program to have desired effects. On the other hand, 41% of nurses (S.E. = 0.08) agreed or strongly agreed that “Coordinating care for complex patients is not compatible with other tasks that I’m required to perform, and only 25% (S.E. = 0.06) that “It is easy for me to coordinate care for complex patients.”
The results of our quasi-experimental study of the effect of implementing a nurse care coordination program in community health centers suggest that adding care coordination to the nursing role is associated with improvement for program enrollees in key program goals, including greater patient access to and engagement with healthcare providers (as indicated by office visit frequency, our implementation indicator) and better patient care experiences ranging from care coordination to care for mental health (key outcome). Moreover, our results indicate that these positive patient effects can occur in a relatively short period following program implementation (6 months), whereas improved clinician teamwork and spillover effects to all high-risk patients may require time. To our knowledge this is the first multi-center study to evaluate the effect of the added-role approach to nurse care coordination on patients’ and staff’s experiences, the early effects, and in community health centers, a setting in which care coordination has been under-studied despite its importance for the vulnerable populations such centers serve. The experience in these low-resource health centers may be informative for other low-resource settings across the world that seek to improve care coordination and patient care experiences. It may also be informative for developed health systems with greater resources as a review of 18 systematic reviews of nurse care coordination in primary care showed uncertainty about the best approach to this role in developed countries (comparable to Australia) as well [ 10 ].
The positive although modest trajectory of effects for program enrollees, particularly in a short timeframe, is notable because uncertainty about the effectiveness of the added-role approach to nurse coordination in particular has prevailed. The question of whether the exclusive-role approach is the only way to garner the benefits of nurse coordination lingered. This study contributes to the literature on care coordination by providing evidence that supports the added-role approach as a potential alternative, if compatibility with other job demands can be cultivated. The results indicate that the effects of this approach, with training and resources provided, are comparable in some respects to larger programs focused on improved care management for high-risk patients. The two-year analysis of the Comprehensive Primary Care Initiative (CPCI) — launched by the U.S. Centers for Medicare and Medicaid Services and 39 other payers and which also used the CG-CAHPS survey to study patient care experience — similarly found a significant but small positive effect on patient self-management [ 60 ]. The more-intensive CPCI required participating primary care practices to build their capacity for care coordination and other skills (e.g., patient engagement) and supported practices by providing them with enhanced payment, data feedback and learning resources [ 60 ]. The CPCI had no significant effect on other aspects of patient care experiences also studied here, including care coordination and timeliness of care.
The results for the added-role approach however mirror larger programs with respect to primary care office visits. A three-percent increase in primary care visits occurred in the first 2 years of the CPCI as well (compared to 5 % here), [ 60 ] and the number of visits increased by 1.3 (same as in this study) in the first six-months of Bridges to Care (B2C)—a hospital-initiated, community-based program [ 53 ]. The consistency in effects across programs is notable because our study differed in population (all adults versus adults ages 65 and older) and setting (community health centers versus primary care practices and hospitals). Although extended study is needed for assessing the degree and persistence of effects found here and therefore to be pursued in future research, these early results are valuable for understanding the trajectory of effects. Moreover, our findings add to research that has found significant effects on care of implementing other types of nursing interventions (e.g., skilled nursing visits in home healthcare) in 6 months [ 48 , 49 , 50 , 53 ].
Greater, short-term improvement in patient care experiences with the added-role approach than we found may be possible under other circumstances. In the centers studied, although leadership made sizable investments in training and infrastructure to support the program, financial constraints limited their ability to provide nurses with extended, protected time for care coordination activities, not unusual in lower-resource settings. Thus, many nurses felt that there was incompatibility between their other job demands and care coordination. Incompatibility can exist because coordination has many components as described in the Intervention section and requires time (e.g., to speak with patients and providers, to schedule care, etc.). When a nurse is focused on coordination tasks for high-risk patients, she or he must reduce the time spent on tasks for other patients, a tradeoff perceived as incompatibility between roles by many nurses. Operations research shows that slack time and flexibility in task timing can be critical for new initiatives, particularly in the early stage of implementation involving role redesign [ 69 , 70 , 71 ]. Larger effects of the added-role approach may emerge if additional time is allotted for coordination activities. The study organization chose the added-role over the exclusive-role approach because nurses felt that non-coordinating nurses would be left with less stimulating work and interactions (e.g., immunizations) and their skills would decline; all nurses wanted involvement in improving care for their neediest patients. An optimal level of involvement in care coordination may require shifting some tasks to other team members (e.g., having medical assistants monitor the list of patients for care coordination) [ 72 ]. With relief from some tasks, allowing nurses more time for care coordination, the added-role approach may be an even better solution for patients and nurses. Thus, our results imply that organizations and health systems using this solution will need to provide protected time for care coordination activities, which may mean changing other workers’ roles. When roles change, it is important that representatives of all affected roles participate in implementation planning to increase consideration of how job components interact and facilitate adjustments in job demands to increase compatibility among roles and thus effectiveness [ 73 ].
There are several possible reasons why clinician teamwork did not increase significantly during the study. One possibility is that more time was needed to improve teamwork. Organizational research on teams has found that teamwork—which involves not only behavioral processes (e.g., collaboration and coordination) but also emergent states that support those processes (e.g., mutual respect and psychological safety that taking interpersonal risks such as asking questions will not be held against you) [ 63 , 74 ]—takes extended time to develop and solidify, [ 75 , 76 ] particularly when compounded by role changes. A literature review found that teams often pass through development phases and try variations in the way they work before they settle into an equilibrated role structure, especially when new members or roles are introduced [ 77 ]. A second possible explanation for the non-significant change is that care coordination is largely a nurse-patient intervention versus a nurse-other clinician intervention in the early phase because nurses work to understand patient circumstances and needs first. A study of non-licensed care coordinators embedded into primary care practices found that these coordinators did not change existing care team functioning, yet patients reported significantly better experiences from these coordinators’ efforts to improve largely nonmedical tasks [ 78 ], which suggests that the coordinator-patient interaction is most central and salient. A third possibility is a ceiling effect: Teamwork was already high (above 3 on the 4-point scale) in all centers, leaving limited room for improvement on the scale. Other potential reasons beyond the three presented here are possible. Ethnographic studies involving direct observation of care teams, interviews of care teams and patients, and sampling of centers for greater variation in teamwork scores are needed to examine the possibilities and better understand changes in teamwork following implementation of nurse care coordination.
We assessed early program impact in part because of project imitations, but also because early effects can be consequential for long-term success [ 43 , 44 , 45 , 46 ]: assessment of early effects allows for managerial intervention if needed to improve program adoption and impact. In addition to the managerial intervention needed to address compatibility between care coordination and other job demands (e.g., implementing protected time and task-shifting between team members), our findings point to the need for managers to plan for an increase in office visits associated with care coordination in the early months (and potentially years). Extended office hours during the week, weekend appointments, and/or additional staffing during existing work hours are potential solutions for increasing capacity to accommodate additional office visits. If funds are not available for these solutions, organizations will need to consider ways to increase efficiency with existing resources to create more time for office visits (e.g., using group visits, electronic communication, etc.). Office visits, especially during the early part of the program, are important because they provide the opportunity for care teams and patients to build rapport and partnership, understand and address care needs that are often complex (requiring physical assessments and conversation), and train patients in self-management. These interactions are key for promoting the “deliberate organization of patient care activities…to facilitate appropriate delivery”, the definition of care coordination” ([ 5 ], p., 5). Not planning for increased visits, alongside training, resources, and compatibility of care coordination with other nurse-job demands is likely to minimize the potential for the added-role approach to build on early progress to produce greater and sustained gains long term.
There are several limitations to our study. First, our results are based on the experiences of patients and staff in a small sample of centers affiliated with one organization in one state. Thus, our results may not generalize to other settings. Second, we were not able to randomize centers to the intervention and control groups. This could result in biased results, although our quasi-experimental design and the similarity in intervention and comparison groups’ characteristics should provide valid insights. Additionally, we adjusted for two observed patient population differences between intervention and comparison sites, and for key patient characteristics. Third, selection bias may have affected our results. Our participation and response rates, however, are comparable or better than other studies of low-income patients [ 69 , 79 ] and clinicians [ 80 ]. Still, it is possible that those who selected to participate differed from those who did not. The latter might report better or worse experiences than participants, which might strengthen or dampen found effects. However, given the modest effects found across the greater than majority of the study population, conclusions likely hold. Finally, we did not assess the full range of experiences that might have been affected (e.g., nurse helpfulness), focusing instead on core measures of patient care experience [ 58 ].
Poor care coordination is a pervasive problem that affects millions of people [ 6 , 81 ] and has been slow to improve, with fewer than half of coordination metrics in the U.S., for example, having improved since 2001 [ 4 ]. Our findings suggest that adding care coordination to the nursing role can spur some improvement in a relatively short time in key metrics, specifically, patient care experiences and accessing care via office visit frequency. With more time, improvement in clinician interactions–from their perspective̶–may be substantial as well. However, compatibility between existing nurse job demands and care coordination needs to be addressed to realize greater benefit from this approach.
Availability of data and materials
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
Agency for Healthcare Research and Quality
Consumer Assessment of Healthcare Providers and Systems Clinician & Group Survey
Federally Qualified Health Center
Bodenheimer T. Coordinating care — a perilous journey through the health care system. New England J Med. 2008;358(10):1064–71.
Article CAS Google Scholar
Institute of Medicine. Priority areas for national action: transforming health care quality. Washington, D.C.: National Academies Press; 2003.
Google Scholar
Institute of Medicine. Best care at lower cost: the path to continuously learning health care in America. Washington, D.C.: National Academies Press; 2013.
Agency for Healthcare Research and Quality. 2015 National healthcare quality and disparities report and 5th anniversary update on the national quality strategy. Rockville, MD: Agency for Healthcare Research and Quality; 2016.
McDonald KM, Sundaram V, Bravata D, Lewis R, Lin N, Kraft S, McKinnon M, Paguntalan H, Owens DK. Care coordination. Closing the quality gap: a critical analysis of quality improvement strategies. In: Shojania KG, KM MD, Wachter RM, Owens DK, editors. vol. 7 technical review 9 (prepared by the Stanford University-UCSF evidence-based practice center under contract 290–02-0017), AHRQ publication no. 04(07)-0051–7. Rockville, MD: Agency for Healthcare Research and Quality; 2007.
Osborn R, Squires D, Doty MM, Sarnak DO, Schneider EC. In new survey of eleven countries, US adults still struggle with access to and affordability of health care. Health Aff. 2016;35:2327–36.
Article Google Scholar
Berwick DM, Hackbarth AD. Eliminating waste in U.S. health care. JAMA. 2012;307(14):1513–6.
Article PubMed Google Scholar
Anderson GF. Medicare and chronic conditions. New England J Med. 2005;353(3):305–9.
National strategy for quality improvement in health care [ http://www.ahrq.gov/workingforquality/ ]. Accessed 3 Nov, 2018.
Parker S, Fuller J. Are nurses well placed as care co-ordinators in primary care and what is needed to develop their role: a rapid review. Health Soc Care Commun. 2016;24(2):113–22.
Al-Qudimat MR, Day S, Almomani T, Odeh D, Qaddoumi I. Clinical nurse coordinators: a new generation of highly specialized oncology nursing in Jordan. J Ped Hematology/Oncology. 2009;31(1):38–41.
Hong CS, Siegel AL, Ferris TG. Caring for high-need, high-cost patients: what makes for a successful care management program? Issue Brief Commonwealth Fund. 2014;19:1–19.
PubMed Google Scholar
Biernacki PJ, Champagne MT, Peng S, Maizel DR, Turner BS. Transformation of care: integrating the registered nurse care coordinator into the patient-centered medical home. Popul Health Manage. 2015;18(5):330–6.
Bauer L, Bodenheimer T. Expanded roles of registered nurses in primary care delivery of the future. Nurs Outlook. 2017;65(5):624–32.
Nutt M, Hungerford C. Nurse care coordinators: definitions and scope of practice. Contemp Nurse. 2010;36(1–2):71–81.
Chen A, Brown R, Archibald N, Aliotta S, Fox P. Best practices in coordinated care. In. Princeton, NJ: Mathematica Policy Research, Inc; 2000.
Camicia M, Chamberlain B, Finnie RR, Nalle M, Lindeke LL, Lorenz L, Hain D, Haney KD, Campbell-Heider N, Pecenka-Johnson K. The value of nursing care coordination: a white paper of the american nurses association. Nurs Outlook. 2013;61(6):490–501.
Institute of Medicine. The future of nursing: leading change, advancing health. Washington, D.C.: National Academies of Sciences; 2011.
Position statement: Care coordination and registered nurses’ essential role [ https://www.nursingworld.org/~4afbf2/globalassets/practiceandpolicy/health-policy/cnpe-care-coord-position-statement-final%2D%2Ddraft-6-12-2012.pdf ]. Accessed 3 Nov, 2018.
Lamb G, Newhouse R. Care coordination: a blueprint for action for RNs. American Nurses Association: Silver Spring, MD; 2018.
Toles M, Moriarty H, Coburn K, Marcantonio S, Hanlon A, Mauer E, Fisher P, O'Connor M, Ulrich C, Naylor MD. Managing chronic illness: nursing contact and participant enrollment in a medicare care coordination demonstration program. J Appl Gerontology. 2017;36(4):462–79.
Haggerty JL, Roberge D, Freeman GK, Beaulieu C, Breton M. Validation of a generic measure of continuity of care: when patients encounter several clinicians. Ann Fam Med. 2012;10:443.
Article PubMed PubMed Central Google Scholar
Haas SA, Swan BA. Developing the value proposition for the role of the registered nurse in care coordination and transition management in ambulatory care settings. Nursing Econ. 2014;32(2):70–9.
Peikes D, Chen A, Schore J, Brown R. Effects of care coordination on hospitalization, quality of care, and health care expenditures among Medicare beneficiaries: 15 randomized trials. JAMA. 2009;301(6):603–18.
Article PubMed CAS Google Scholar
Nelson L. Lessons from Medicare’s demonstration projects on care coordination. In. Congressional Budget Office: Washington, D.C; 2012.
Bosch M, Faber MJ, Cruijsberg J, Voerman GE, Leatherman S, Grol RPTM, Hulscher M, Wensing M. Review article: effectiveness of patient care teams and the role of clinical expertise and coordination: a literature review. Med Care Res Rev. 2009;66(6 suppl):5S–35S.
Conway A, O’Donnell C, Yates P. The effectiveness of the nurse care coordinator role on patient-reported and health service outcomes: A systematic review. Eval Health Prof. 2017; online ahead of print.
Marek KD, Popejoy L, Petroski G, Rantz M. Nurse care coordination in community-based long-term care. J Nursing Scholarship. 2006;38(1):80–6.
Peikes D, Peterson G, Brown RS, Graff S, Lynch JP. How changes in Washington University’s Medicare coordinated care demonstration pilot ultimately achieved savings. Health Aff. 2012;31(6):1216–26.
Schore J, Peikes D, Peterson G, Gerolamo A, Brown R. Fourth report to Congress on the evaluation of the Medicare coordinated care demonstration. Mathematica Policy Research; 2011.
Verhaegh KJ, MacNeil-Vroomen JL, Eslami S, Geerlings SE, de Rooij SE, Buurman BM. Transitional care interventions prevent hospital readmissions for adults with chronic illnesses. Health Aff. 2014;33(9):1531–9.
Naylor MD, Aiken LH, Kurtzman ET, Olds DM, Hirschman KB. The importance of transitional care in achieving health reform. Health Aff. 2011;30(4):746–54.
Coleman EA, Parry C, Chalmers S. Min S-j. the care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166(17):1822–8.
Boyd CM, Reider L, Frey K, Scharfstein D, Leff B, Wolff J, Groves C, Karm L, Wegener S, Marsteller J. The effects of guided care on the perceived quality of health care for multi-morbid older persons: 18-month outcomes from a cluster-randomized controlled trial. J Gen Intern Med. 2010;25(3):235–42.
Doty MM, Fryer A, Audet A. The role of care coordinators in improving care coordination: the patients' perspective. Arch Intern Med. 2012;172(7):587–8.
Brown R. The promise of care coordination: models that decrease hospitalizations and improve outcomes for Medicare beneficiaries with chronic illnesses. A report commissioned by the National Coalition on Care Coordination (N3C). Princeton: Mathematica Policy Research; 2009.
Xing J, Goehring C, Mancuso D. Care coordination program for Washington state Medicaid enrollees reduced inpatient hospital costs. Health Aff. 2015;34(4):653–61.
Davis K, Schoenbaum SC, Audet AM. A 2020 vision of patient-centered primary care. J Gen Intern Med. 2005;20(10):953–7.
Shi L, Lebrun LA, Tsai J, Zhu J. Characteristics of ambulatory care patients and services: a comparison of community health centers and physicians' offices. J Health Care Poor Underserved. 2010;21(4):1169–83.
Powers BW, Chaguturu SK, Ferris TG. Optimizing high-risk care management. JAMA. 2015;313(8):795–6.
McWilliams JM, Chernew ME, Landon BE. Medicare ACO program savings not tied to preventable hospitalizations or concentrated among high-risk patients. Health Aff. 2017;36(12):2085–93.
Alexander JA, Hearld LR. The science of quality improvement implementation: Developing capacity to make a difference. Med Care. 2011;49(Supplement):S6–S20.
Sterman JD, Repenning NP, Kofman F. Unanticipated side effects of successful quality programs: exploring a paradox of organizational improvement. Manag Sci. 1997;43(4):503–21.
Keating E, Oliva R, Repenning N, Rockart S, Sterman J. Overcoming the improvement paradox. European Management J. 1999;17(2):120–34.
Burns LR, Pauly MV. Integrated delivery networks: a detour on the road to integrated health care? Health Aff. 2002;21(4):128–43.
Pisano GP, Bohmer RMJ, Edmondson AC. Organizational differences in rates of learning: evidence from the adoption of minimally invasive cardiac surgery. Manag Sci. 2001;47(6):752–68.
Fiske ST, Taylor SE. Social cognition. 2nd ed. New York: McGraw-Hill; 1991.
O’Connor M, Bowles KH, Feldman PH, St. Pierre M, Jarrín O, Shah S, Murtaugh CM. Frontloading and intensity of skilled home health visits: a state of the science. Home Health Care Services Quart. 2014;33(3):159–75.
O'Connor M, Hanlon A, Bowles KH. Impact of frontloading of skilled nursing visits on the incidence of 30-day hospital readmission. Geriatr Nurs. 2014;35(2):S37–44.
Rogers J, Perlic M, Madigan EA. The effect of frontloading visits on patient outcomes. Home Healthcare Now. 2007;25(2):103–9.
Primary care medical home [ https://www.jointcommission.org/accreditation/pchi.aspx ]. Accessed 3 Nov, 2018.
Patient-centered medical home [ https://www.ncqa.org/programs/health-care-providers-practices/patient-centered-medical-home-pcmh/ ]. Accessed 3 Nov, 2018.
Capp R, Misky GJ, Lindrooth RC, Honigman B, Logan H, Hardy R, Nguyen DQ, Wiler JL. Coordination program reduced acute care use and increased primary care visits among frequent emergency care users. Health Aff. 2017;36(10):1705–11.
Dopson S, Fitzgerald L. The active role of context. In: Dopson S, Fitzgerald L, editors. Knowledge to action? Evidence-based health care context. Oxford: Oxford University Press; 2006. p. 223.
Damschroeder LJ, Aron DC, Keith RE, Kirsch SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Sci. 2009;4:50.
Dyer N, Sorra JS, Smith SA, Cleary PD, Hays RD. Psychometric properties of the Consumer Assessment of Healthcare Providers and Systems (CAHPS®) Clinician and Group Adult Visit Survey. Med Care. 2012;50(Suppl):S28–34.
CAHPS Clinician & Group Survey. Content last reviewed March 2019. Rockville: Agency for Healthcare Research and Quality. http://www.ahrq.gov/cahps/surveys-guidance/cg/index.html . Accessed 3 Nov 2018.
Scholle SH, Vuong O, Ding L, Fry S, Gallagher P, Brown JA, Hays RD, Cleary PD. Development of and field test results for the CAHPS PCMH survey. Med Care. 2012;50(Suppl):S2–10.
Anhang Price R, Elliott MN, Zaslavsky AM, Hays RD, Lehrman WG, Rybowski L, Edgman-Levitan S, Cleary PD. Examining the role of patient experience surveys in measuring health care quality. Med Care Res Rev. 2014;71(5):522–54.
Dale SB, Ghosh A, Peikes DN, Day TJ, Yoon FB, Taylor EF, Swankoski K, O’Malley AS, Conway PH, Rajkumar R, et al. Two-year costs and quality in the Comprehensive Primary Care Initiative. New Engl J Med. 2016;374(24):2345–56.
Martino SC, Elliott MN, Hambarsoomian K, Weech-Maldonado R, Gaillot S, Haffer SC, Hays RD. Racial/ethnic disparities in Medicare beneficiaries' care coordination experiences. Med Care. 2016;54(8):765–71.
Hoegl M, Gemuenden HG. Teamwork quality and the success of innovative projects: a theoretical concept and empirical evidence. Organ Sci. 2001;12(4):435–49.
Valentine MA, Nembhard IM, Edmondson AC. Measuring teamwork in health care settings: a review of survey instruments. Med Care. 2015;53(4):e16–30.
Salas E, Wilson KA, Murphy CE, King H, Salisbury M. Communicating, coordinating, and cooperating when lives depend on it: tips for teamwork. Jt Comm J Qual Patient Saf. 2008;34(6):333–41.
Nembhard IM, Tucker AL. Deliberate learning to improve performance in dynamic service settings: evidence from hospital intensive care units. Organization Sci. 2011;22(4):907–22.
Gittell JH. Coordinating mechanisms in care provider groups: relational coordination as a mediator and input uncertainty as a moderator of performance effects. Manag Sci. 2002;48(11):1408–25.
Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Quart. 2003:425–78.
Zaslavsky AM, Zaborski LB, Ding L, Shaul JA, Cioffi MJ, Cleary PD. Adjusting performance measures to ensure equitable plan comparisons. Health Care Financ Rev. 2001;22(3):109–26.
PubMed PubMed Central Google Scholar
Zlateva I, Anderson D, Coman E, Khatri K, Tian T, Fifield J. Development and validation of the medical home care coordination survey for assessing care coordination in the primary care setting from the patient and provider perspectives. BMC Health Serv Res. 2015;15:226.
Zinn J, Flood AB. Commentary: slack resources in health care organizations—fat to be trimmed or muscle to be exercised? Health Serv Res. 2009;44(3):812–20.
Mohr DC, Young GJ. Slack resources and quality of primary care. Med Care. 2012;50(3):203–9.
Friedman A, Howard J, Shaw EK, Cohen DJ, Shahidi L, Ferrante JM. Facilitators and barriers to care coordination in patient-centered medical homes (PCMHs) from coordinators' perspectives. J Amer Board Fam Med. 2016;29(1):90–101.
Nembhard IM, Morrow CT, Bradley EH. Implementing role-changing versus time-changing innovations in health care: differences in helpfulness of staff improvement teams, management, and network for learning. Med Care Res Rev. 2015;72(6):707–35.
Ilgen DR, Hollenbeck JR, Johnson M, Jundt D. Teams in organizations: from input-process-output models to imoi models. Ann Rev Psychol. 2005;56(1):517–43.
O’Malley A, Gourevitch R, Draper K, Bond A, Tirodkar M. Overcoming challenges to teamwork in patient-centered medical homes: a qualitative study. J Gen Intern Med. 2015;30(2):183–92.
Rousseau V, Aubé C, Savoie A. Teamwork behaviors: a review and an integration of frameworks. Small Group Res. 2006;37(5):540–70.
Arrow H, Poole MS, Henry KB, Wheelan S, Moreland R. Time, change, and development: the temporal perspective on groups. Small Group Res. 2004;35(1):73–105.
Di Capua P, Clarke R, Tseng CH, Wilhalme H, Sednew R, McDonald KM, Skootsky SA, Wenger N. The effect of implementing a care coordination program on team dynamics and the patient experience. Am J Manag Care. 2017;23(8):494–500.
Fredrickson DD, Jones TL, Molgaard CA, Carman CG, Schukman J, Dismuke SE, Ablah E. Optimal design features for surveying low-income populations. J Health Care Poor Underserved. 2005;16(4):677–90.
McLeod CC, Klabunde CN, Willis GB, Stark D. Health care provider surveys in the United States, 2000-2010: a review. Eval Health Prof. 2013;36(1):106–26.
Ward BW, Schiller JS, Goodman RA. Multiple chronic conditions among us adults: a 2012 update. Prev Chronic Dis. 2014;11:E62.
Download references
Acknowledgements
The authors thank Carol Cosenza, Lee Hargraves, and colleagues at the Center for Survey Research at University of Massachusetts – Boston for assistance with CG-CAHPS survey administration; Khushbu Khatri, Thomas Meehan, and Tierney Giannotti of Community Health Center, Inc. for on-site research assistance; and Dava Flowers-Poole and Tessa Chu for general research assistance. This research was presented at the AcademyHealth Annual Research Meeting.
This research was funded by a Cooperative Agreement from the Agency for Healthcare Research and Quality (AHRQ; U18 HS016978: PI: Paul Cleary, PhD) as part of the Consumer Assessment of Healthcare Providers and Systems (CAHPS) program. The funding agency played no role in any aspect of this study. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agency.
Author information
Authors and affiliations.
The Wharton School, University of Pennsylvania, Health Care Management Department, 3641 Locust Walk, 207 Colonial Penn Center, Philadelphia, PA, 19104, USA
Ingrid M. Nembhard
Yale Center for Analytical Sciences (YCAS), 300 George Street, Suite 555, New Haven, CT, 06519, USA
Eugenia Buta
Columbia University Mailman School of Public Health, Department of Health Policy & Management, 722 West 168th Street, R476, New York, NY, 10032, USA
Yuna S. H. Lee
Weitzman Institute, Community Health Center, Inc., 631 Main St., Middletown, CT, 06457, USA
Daren Anderson & Ianita Zlateva
Yale School of Public Health, 60 College St., P.O. Box 208034, New Haven, CT, 06520-8034, USA
Paul D. Cleary
You can also search for this author in PubMed Google Scholar
Contributions
IMN and PDC were involved in all aspects of the study and manuscript development. EB analyzed and interpreted the data, and revised for important statistical content. YSL, DA and IZ made substantial contributions to the conception and design of the data, facilitated data collection, and revised the manuscript critically for important intellectual content. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Corresponding author
Correspondence to Ingrid M. Nembhard .
Ethics declarations
Ethics approval and consent to participate.
This study was approved by the Yale University Human Investigations Committee (Application number: 1204010010) and the institutional review board of the FQHC. Participating health professionals completed a consent form. Patients provided verbal consent at the time of survey administration.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License ( http://creativecommons.org/licenses/by/4.0/ ), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated.
Reprints and permissions
About this article
Cite this article.
Nembhard, I.M., Buta, E., Lee, Y.S.H. et al. A quasi-experiment assessing the six-months effects of a nurse care coordination program on patient care experiences and clinician teamwork in community health centers. BMC Health Serv Res 20 , 137 (2020). https://doi.org/10.1186/s12913-020-4986-0
Download citation
Received : 31 December 2018
Accepted : 09 October 2019
Published : 24 February 2020
DOI : https://doi.org/10.1186/s12913-020-4986-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Nurse care coordination
- Patient care experience
BMC Health Services Research
ISSN: 1472-6963
- General enquiries: [email protected]
ORIGINAL RESEARCH article
Impact of weekly physical activity on stress response: an experimental study.

- 1 Department of Physical Education, Sport and Human Movement, Autonomous University of Madrid, Madrid, Spain
- 2 Didactic and Behavioral Analysis in Sport Research Group, Faculty of Sport Sciences, University of Extremadura, Cáceres, Spain
- 3 Sport of Studies Center, Rey Juan Carlos University, Madrid, Spain
The aim of this research is focused on analyzing the alteration of the psychophysiological and cognitive response to an objective computerized stress test (Determination Test - DT-, Vienna test System ® ), when the behavioral response is controlled. The sample used was sports science students (N = 22), with a mean age of 22.82 (M age = 22.82; SD years = 3.67; M PhysicalActivity hours/Week = 7.77; SD hours / week = 3.32) A quasi-experimental design was used in which the response of each participant to the DT test was evaluated. The variable “number of hours of physical activity per week” and the variable “level of behavioral response to stress” were controlled. Before and after this test, the following parameters were measured: activation and central fatigue (Critical Flicker Fusion Threshold (CFF Critical flicker fusion ascending and Critical flicker fusion descending; DC potential), and perceived exertion (Central Rating of Perceived Exertion and Peripheral Rating of Perceived Exertion). Significant differences were found in all of the measures indicated. The usefulness of this protocol and the measures used to analyze the stress response capacity of the study subjects are discussed.
Introduction
The analysis of psychophysiological fatigue is considered very important in different contexts ( Lohani et al., 2019 ). In this sense, the consideration of the study of humans’s response to external and internal loads ( Wijesuriya et al., 2007 ; Wilson et al., 2007 ) has become one of the most important research topics. The external loads exerted on the individual are added to their skills and coping strategies, resulting in a level of tolerance and adaptation to each situation ( Folkman and Lazarus, 1988 ). Along the last decades, distinctions are often made between physical and mental fatigue role, indicating clear methodologies for the analysis of physiological fatigue, but with clear limitations in the study of central fatigue, because this is measurable only indirectly, which emphasizes the importance of developing new central fatigue analysis procedures ( Bittner et al., 2000 ).
Throughout the decades of research on this topic, different strategies have been used to evaluate the adaptation to these external and internal loads ( Lazarus, 1990 ; Amann, 2011 ). Thus, for example, a multitude of self-reports and standardized tests have been used ( Britner et al., 2003 ), to which physiological and biological measures have been added ( Arza et al., 2019 ). However, relatively low attention is usually given to the Central Nervous System (CNS)-related mechanisms, which play a major role on the development of fatigue ( Tarvainen et al., 2014 ), but are rarely monitored in the sport and physical activity field ( Valenzuela et al., 2020 ). Most of the studies related to central fatigue to date have focused on the effect it has on performing strenuous physical tasks ( Amann and Dempsey, 2008 ), although over the last few years there has been a notable increase in interest in studying the role of central fatigue in explaining human performance ( Inzlicht and Marcora, 2016 ). In this sense, the psychobiological model based on motivational intensity theory has gained special strength ( Gendolla and Richter, 2010 ). This model emphasizes that perception of effort and potential motivation are the central determinants of task engagement. Both variables are taken into consideration in our research, controlling the involvement in the task (motivation), by applying a computerized test, and analyzing the perception of both central and peripheral effort as detailed in the methodological section.
Two of these measures, which focus the methodological attention of this research due to its great potential in the study of this topic, are the Critical Flicker Fusion Threshold (CFFT), evaluated using one Flicker Fusion instrument ( Vicente-Rodríguez et al., 2020 ), and the DC Potential, evaluated using the OmegaWave technology. The neuro-physiological basis of flicker perception is complex but well established ( Görtelmeyer and Zimmermann, 1982 ). In particular, flickering light directly influences cortical activity. The CFFT was measured using two red light- emitting diodes in binocular foveal fixation. The continuous psychophysical method of limits was employed to determine CFFT ( Woodworth and Schlosberg, 1954 ). The utility of CFFT in sport has been focused on the relationship of arousal level with CNS ( Görtelmeyer and Zimmermann, 1982 ). Increase in CFFT suggests an increase in cortical arousal and sensory sensitivity. By contrast, a decrease of CFFT suggests a reduction in the efficiency of the system to process information ( Li et al., 2004 ; Clemente and Díaz, 2019 ). On the other hand, for the evaluation of the brain’s direct current (DC) potentials -slow potentials that reflect alterations in brain excitability- OmegaWave technology has gained strength in recent years ( Naranjo-Orellana et al., 2020 ; Valenzuela et al., 2020 ). This device not only measures the Heart Rate Variability (HRV) but it also simultaneously a brainwave signal (DC potential) in order to complement the information obtained from HRV to assess the athlete’s functional state ( Naranjo-Orellana et al., 2020 ). DC potentials—frequency ranges between 0 and 0.5 Hz, are correlated with different brain processes, such as take consciousness during decision making ( Guggisberg and Mottaz, 2013 ) high alertness states ( Bachmann, 1984 ), arousal state ( Haider et al., 1981 ), or attention ( Rösler et al., 1997 ).
To date, most studies conducted in the evaluation of central fatigue have shown that the greatest disturbances are produced by tasks that require efforts at maximum speed that involve a large amount of force ( Davranche and Pichon, 2005 ; Clemente and Díaz, 2019 ). However, there are very few studies that have analyzed central fatigue through controlled analysis of a task that primarily involves central fatigue ( Fuentes et al., 2019 ). In this sense, the aim is to apply a computerized test (DT, Vienna Test System), that allows evaluating people’s tolerance to stress and central fatigue by applying a standardized protocol, in physical activity practitioners. The knowledge in this field is really limited, for this reason we developed the present research with the aim of studying the modifications in CFFT and DC potentials in a sample group of regular physical activity. The first hypothesis establishes that the computerized stress task increases the participants’ perception of central fatigue, while keeping the perception of peripheral fatigue stable. As a consequence, the second hypothesis establishes that differences will be found in the “post” situation in the CFFT measures and in the central physiological indicators, which would indicate a relationship between the subjective and objective measures of central fatigue.
Materials and Methods
This study followed a quasi-experimental design ( Montero and León, 2007 ) and it received the approval of the University Ethical Commission in compliance with the Helsinki Declaration. All subjects were informed about the procedure and gave their written consent to participate. This study was carried out complying with the Standards for Ethics in Sport and Exercise Science Research ( Harriss et al., 2019 ).
Participants
The participants included 22 individuals from Madrid (Spain), 18 of whom were male and 4 females. These participants were aged between 18 and 36 years ( M years = 22.82, SD years = 3.67). All of the participants regularly engaged in physical activity, between 4 and 14 h per week ( M hours / week = 7.77, SD hours / week = 3.32). The inclusion criteria was that they performed physical activity at least 3 times a week and 150 min of moderate/vigorous physical activity. The exclusion criteria was not correctly performing the proposed measurements. Four participants were excluded from the study for not completing the measurements correctly. Intentional sampling methods were used ( Montero and León, 2007 ). Due to the impossibility of continuing with the data collection due to the Alert State decreed by the Spanish Government as a result of COVID-19, the sample had to be closed with the participants who had passed all the tests before March 2020.
Instrumentation and Study Variables
The number of hours of physical activity per week and the scores obtained on the DT test were used as controlled variables. This allows us to know that the differences found are not due to the ability to respond to stress, or to the weekly amount of physical exercise performed. Therefore, only the subjects in which there were no statistically significant differences in their weekly level of physical exercise, nor in the scores obtained in the DT test, were used.
To carry out this research, three measurement systems have been used: OmegaWave device, Flicker Fusion Unit (Vienna Test System), and the Determination Test (Vienna Test System). OmegaWave is a device that assesses the physiological readiness of athletes by examining the autonomic balance through HRV and brain‘s energy balance via DC potential ( Gómez-Oliva et al., 2019 ), Elastic chest band MEDITRACE (dominant hand and forehead). Coach + application (OmegaWave Ltd, Espoo, Finland) was used on Ipad mini 2 32GB. The Vienna Test System is an instrument for computerized psychological assessments that allows the objective evaluation of different psychological parameters. The Determination Test (DT Vienna test system) ( Whiteside, 2002 ; Whiteside et al., 2003 ) was used to determine neuropsychological fatigue. The test studied the attentional capacity, reactive stress tolerance, reaction speed among continuously, and quickly changing acoustic and visual stimuli. The test is simple, the difficulty of the task lies in the different modality of the arriving stimuli and their speed. This way we measure those cognitive abilities of the people involved that are needed for the distinction of colors and sounds, the perception of the characteristics of stimuli, their memorization, and finally, the selection of the adequate answer. The stimuli coming during the test are not predictable. Instead, the subjects need to react to them randomly ( Schuhfried, 2013 ). We study four key variables: the average value of reaction speed (sec), the number of correct answers (raw score), which reflects the ability of the respondent to precisely and quickly select the adequate answer even under pressure. Furthermore, we also examine the number of incorrect answers (raw score) which can show us how likely the respondent is to get confused under stress and pressure; finally, the high number of missed answers (raw score) reveals that the respondent is not capable of maintaining his/her attention under stress and is prone to giving up these situations ( Neuwirth and Benesch, 2012 ). The duration of this test was 6 min.
Before and after the stress test the following parameters were analyzed in this order:
Parameters analyzed through OmegaWave Coach + device ® (OmegaWave Ltd, Espoo, Finland):
– Hear Rate Variability (HRV). Square root of the mean of the squares of successive RR interval differences (RMSSD), Standard deviation of all normal to normal RR intervals (SDNN), and Standard deviation of successive squares of intervals RR (SDSD). OmegaWave is a device that assesses the physiological readiness of athletes by examining autonomic balance through HRV and brain‘s metabolic state via DC potential ( Ilyukhina and Zabolotskikh, 2020 ). Elastic chest band MEDITRACE (dominant hand and forehead). Coach + application (Omegawave Ltd., Espoo, Finland) was used on Ipad mini 2 32GB. For calculating HRV it be used the Root Mean Square of the Successive Differences score (RMSSD) ( Ilyukhina et al., 1982 ). It was used before and after the stress test.
– DC potential dynamics. DC Potential represent changes in the brain’s metabolic balance in response to increased exercise intensity or psychological challenges and are linked to cognitive and mental load ( Wagshul et al., 2011 ; Ilyukhina, 2015 ).
– CNS System Readiness ( Ilyukhina, 1986 ). It’s indicated by a floating grade from 1.0 to 7.0, where 7.0 is the optimal state. This index represents the state of the brain’s energy level and is composed of three factors (in order of significance): stabilization point of DC potential (mV), stabilization time (reduces system readiness state of 1.0–7.0, if not optimal), and curve shape (reduces system readiness state of 1.0–7.0, if not optimal).
– Stabilization point of DC Potential (mV) ( Ilyukhina et al., 1982 ; Ilyukhina, 2013 ): The first priority in DC analysis is the stabilization point of DC Potential. In the literature, especially by Ilyukhina, this point is defined as Level of Operational Rest. In 1982, the combined work of Ilyukhina and Sychev was published which outlined quantitative parameters of LOR for the assessment of the healthy human’s adaptation and compensatory−adaptive abilities to physical and mental loads in sports.
– Stabilization time ( Ilyukhina and Zabolotskikh, 1997 ). The second priority of analysis is to look at the stabilization time. measured in minutes. The spontaneous relaxation speed represents neuroreflex reactivity (neural control of baroreflex arch) of cardiovascular and respiratory systems. This measure associated with psycho-emotional dynamic and stability. Normal stabilization time occurs within 2 min and represents optimal balance within stress-regulation systems.
– Curve Shape: The curve shape is composed of two elements: Difference between measurement start mV and end mV values ( Table 1 ). The optimal shape of the curve should show a smooth transition from a higher initial value (active wakefulness) to a lower stabilization value (operational rest DC potential form represents the dynamic interaction within stress-regulation systems). DC potential form can indicate the level of CNS activation balance.
Parameters analyzed though Flicker Fusion unit (Vienna Test System ® ):
– Critical flicker fusion ascending (Hz) (CFFA) and Critical flicker fusion descending (Hz) (CFFD). Cortical arousal was measured using the critical flicker fusion threshold (Hz) (CFFT) in a viewing chamber (Vienna Test System ® ), following the procedure of previous studies ( Clemente et al., 2016 ). An increase in CFFT suggests an increase in cortical arousal and information processing; a decrease in CFFT values below the baseline reflects a reduction in the efficiency of information processing and central nervous system fatigue ( Whiteside, 2002 ). It was used before and after the stress test.
Parameters analyzed though DT test (Vienna Test System ® ):
– We study four key variables: the average value of reaction speed (msec), the number of correct answers (raw score), which reflects the ability of the respondent to precisely and quickly select the adequate answer even under pressure. Furthermore, we also examine the number of incorrect answers (raw score) which can show us how likely the athlete is to get confused under stress and pressure; finally, the high number of missed answers (raw score) reveals that the respondent is not capable of maintaining his/her attention under stress and is prone to giving up these situations ( Neuwirth and Benesch, 2012 ). The duration of this test was 6 min without instructions.
Parameters analyzed by self-report instruments:
– Central Rating of Perceived Exertion (RPEC) and Peripheral Rating of Perceived Exertion (RPEP). The Rating of Perceived Exertion ( Borg, 1998 ), was used as a measure of central (cardiorespiratory) and peripheral (local-muscular, metabolic) exertion before and after the stress test ( Bolgar et al., 2010 ; Cárdenas et al., 2017 ). The RPE is a 15 point category-ratio; the odd numbered categories have verbal anchors. Beginning at 6, “no exertion at all,” and goes up to 20, “maximal exertion.” Before testing, subjects were instructed on the use of the RPE scale ( Noble and Robertson, 1996 ). We use the scale with the clear differentiation between central as peripheral perceived exertion following the recommendations of the medical staff and under the guideline of Borg ( Borg, 1982 ), for applied studies.
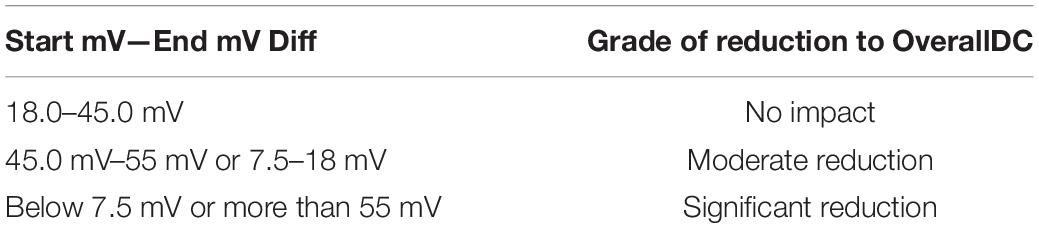
Table 1. Simplified curve change mV reduction algorithm.
The participants were contacted and informed about the measurement protocol and of the date and time of the data collection. All of the measurements were collected during the same day. The total data collection time per participant was approximately 45 min. The order of measurements was the following: CFFT, DC Potential, RPE, DT test, RPE, CFFT, and DC Potential.
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 21 (SPSS Inc., Chicago, Ill., United States). Means and SDs were calculated using traditional statistical techniques. Normality was tested with the Shapiro-Wilk test. As the distributions were not adjusted to the normal, non-parametric tests were used. A Wilcoxon sign ranges test for intragroup comparisons were conducted to analyze differences between pre and post-test. A Rho Spearman coefficient was used to know the correlations between variables. The Effect Size was tested using the formula = Z/ N for non-parametric tests ( Tomczak and Tomcak, 2014 ). Following the considerations of Cohen (1988) , the effect size is considered small when the value is inferior to 0.10, medium when it varies between 0.10 and 0.30 and high when it is superior to 0.50. The significance level was set at p < 0.05.
Descriptive Analysis, Normality Test According N, Wilcoxon Test, and Effect Sizes
Firstly, the normality tests were realized with the Shapiro-Wilk test. It was determined that most of the variables were not normal, due to which non-parametric statistical tests were applied. In relation to the descriptive analyzes of the study variables, shown in Table 2 , after applying the stressor via the DT test, worse values were obtained in all the variables measured. This reflects the alterations in the central response evaluated. Regarding the Wilcoxon rank test that was used to analyze whether there were differences between the scores obtained before and after applying the stressor (DT test), significant differences were found in the variables OverallDc ( p < 0.05), Flicker ascending ( p < 0.01), Flicker descending ( p < 0.01), Central RPE ( p < 0.01) and Physical RPE ( p < 0.01), while not finding significant differences in the rest of the variables ( Table 2 ).
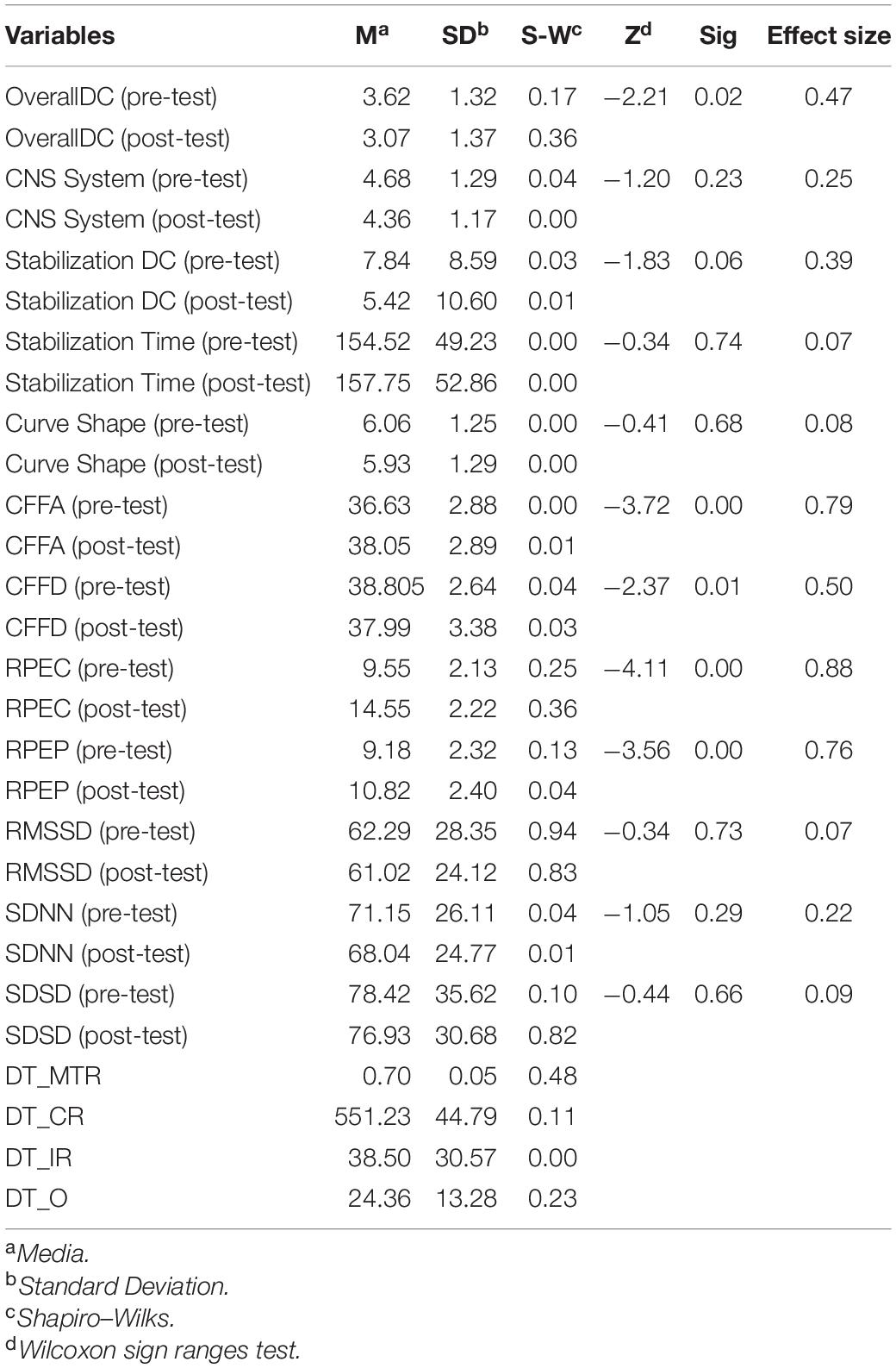
Table 2. Descriptive analysis of the measured variables.
Correlation Analysis
A Spearman bivariate correlation analysis was performed. Spearman’s Rho coefficient was used, since the distribution was non-parametric. Note that significant correlations were found ( Table 3 ) entre OverallDC con DCSSatabilizationLevel ( p = 0.000; r = 0.791 ∗∗ ); OWCNS ( p = 0.005; r = 0.581 ∗∗ ); OWDCC ( p = 0.013; r = 0.522 ∗ ); Flicker Descending ( p = 0.044; r = 0.432 ∗ ). DCSStabilizationLevel con OWCNS ( p = 0.000; r = 0.766 ∗∗ ); Flicker Descending ( p = 0.049; r = 0.424 ∗ ). DCSStabilizationTime con OWCNS ( p = 0.005; r = 0.572 ∗ ); OWDCC ( p = 0.046; r = 0.430 ∗ ); Flicker Ascending ( p = 0.006; r = 0.563 ∗∗ ). OWCNS correlated with Flicker Ascending ( p = 0.018; r = 0.499 ∗ ), and SDSD with Flicker Descending score ( p = 0.046; r = −0.430 ∗ ).
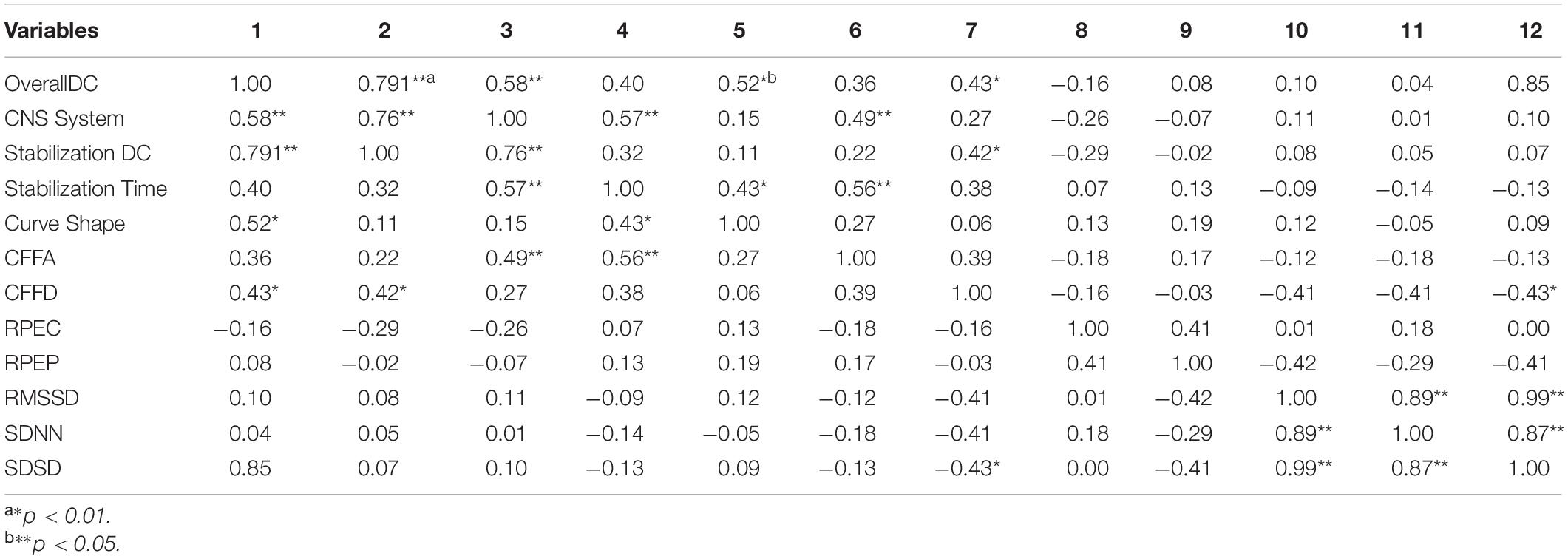
Table 3. Rho Spearman coefficient.
The objective of the present research was to study the modification of DC potentials and the CFFT scores after the computerized stress test (DT). The analysis of the subjective cognitive responses about fatigue after DT test reveals significant differences in the participants, both at a physical and central level. As regards the first hypothesis, it is partially fulfilled. There are significant differences in central perceived fatigue, with a very high effect size, which supports the hypothesis and emphasizes the usefulness of the established research protocol. However, significant differences also appear in peripheral perceived fatigue, which is beyond the initial approaches. This result is of special interest because it allows to consider the relationship between both types of perceived fatigue ( Bittner et al., 2000 ; Clemente et al., 2016 ). These results, taking into account that the participants did the test sitting down, emphasize the effect achieved through the protocol used to generate stress in them, without significant differences in the performance achieved in the task. Previous research carried out with the DT test already points in this same direction ( Ong, 2015 ). The differences found in the perception of physical fatigue even without previous movement are interesting. Similar results are found in studies carried out in contexts such as chess ( Fuentes et al., 2019 ), where central fatigue due to the demands of each game also leads to physical fatigue of the players. This fact seems relevant insofar as the studies should incorporate measures of both dimensions to be able to explain a higher percentage of variance of the results found.
As regards the second hypothesis, the decrease of CFFD values indicates that it has a negative effect generating central fatigue and an alteration in cortical activation ( Li et al., 2004 ; Clemente, 2016 ). These results confirm the alterations in cortical activation found in physiological efforts of high intensity and of short duration, such as sprints at maximum speed ( Clemente et al., 2011 ). This same trend is also observed in research focused on generating a high level of stress in soldiers, which emphasizes the usefulness of using the DT test to create stress in the participants ( Clemente et al., 2016 ). In line with the ideas defended by Clemente (2016) , decreased in CFFD scores seem to be linked to high sympathetic autonomous nervous system activation, which could also affect higher cognitive functions, such as executive processes (i.e., making complex decisions, memory, and attention processes) ( Shields et al., 2016 ). These same considerations can also be made with respect to the significant differences found in CFFA scores. Higher scores are found after the stress test, which implies that the participants have needed more time to respond to the flicker task as consequence of central fatigue ( Fuentes et al., 2019 ; Lohani et al., 2019 ).
Regarding the results obtained in the Overall DC scores, the significant differences show a pattern of alteration as a consequence of the stress test. As Naranjo-Orellana et al. (2020) point out, the OW test obtains good reliability and validity values using the heart rate variability as a measure in conjunction with the DC Potential (stabilitation DC, stabilitation time, and curve shape). Changes in the DC potentials have been reported to be reflective of performance in different brain processes ( Haider et al., 1981 ; Valenzuela et al., 2020 ). The lower scores obtained after the stress test could indicate, as with the CFF scores, an increase in central fatigue detected by the OmegaWave system ( Valenzuela et al., 2020 ). This result, in any case, needs to be analyzed in detail in future research.
Therefore, monitoring the DC potentials and the CFF scores could be useful to control the cognitive load of the different tasks that having a high mental demand.
Due to the exceptional circumstances of data collection in the present study, some of the study limitations were the sample size and the small number of women who participated in it. Future research works should expand the sample power, as well as determine its effect in a sedentary sample.
To conclude, this is the first study that has jointly analyzed the scores obtained in the analysis of low-frequency brain waves (DC potentials), together with those obtained in the Flicker test. In this sense, although the performance in a specific task seems similar, the demand it has for the person must be evaluated, being useful the use of research protocols similar to the ones we have used. The results open a new field where both measurements could be interesting and useful to assess the cognitive demands of persons.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation, to any qualified researcher.
Ethics Statement
The studies involving human participants were reviewed and approved by the University Ethical Commission in compliance with the Helsinki Declaration. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
RV: conceptualization, investigation, resources, writing—review and editing, and project administration. RV, ML-R, and RJ-C: methodology, data curation, writing—original draft preparation, visualization, supervision, and formal analysis. ML-R and RJ-C: software and validation.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Amann, M. (2011). Central and peripheral fatigue: interaction during cicling exercise in humans. Med. Sci. Sports Exerc. 43, 2039–2045. doi: 10.1249/MSS.0b013e31821f59ab
PubMed Abstract | CrossRef Full Text | Google Scholar
Amann, M., and Dempsey, J. A. (2008). Locomotor muscle fatigue modifies central motor drive in healthy humans and imposes a limitation to exercise performance. J. Physiol. 586, 161–173. doi: 10.1113/jphysiol.2007.141838
Arza, A., Garzón-Rey, J. M., Lázaro, J., Gil, E., López-Anton, R., de la Cámara, C., et al. (2019). Measuring acute stress response through physiological signals: towards a quantitative assessment of stress. Med. Biol. Eng. Comput. 57, 271–287. doi: 10.1007/s11517-018-1879-z
Bachmann, T. (1984). The process of perceptual retouch: nonspecific afferent activation dynamics in explaining visual masking. Percept. Psychophys. 35, 69–84. doi: 10.3758/BF03205926
Bittner, R., Hána, K., Pousek, L., Smrka, P., Schreib, P., and Vysoky, P. (2000). “Detecting of fatigue states of a car driver,” in Medical Data Analysis. ISMDA 2000. Lecture Notes in Computer Science , Vol. 1933, eds R. W. Brause and E. Hanisch (Berlin: Springer).
Google Scholar
Bolgar, M. R., Baker, C. E., Goss, F. L., Nagle, E., and Robertson, R. J. (2010). Effect of exercise intensity on differentiated and undifferentiated ratings of perceived exertion during cycle and treadmill exercise in recreationally active and trained women. J. Sports Sci. Med. 9, 557–563.
Borg, G. (1982). Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 14, 377–381. doi: 10.1249/00005768-198205000-00012
Borg, G. (1998). Perceived Exertion and Pain Scale. Champaign, IL: Human Kinetics.
Britner, P. A., Morog, M. C., Pianta, R. C., and Marvin, R. S. (2003). Stress and coping: a comparison of self-report measures of functioning in families of young children with cerebral palsy or no medical diagnosis. J. Child Fam. Stud. 12, 335–348. doi: 10.1023/A:1023943928358
CrossRef Full Text | Google Scholar
Cárdenas, D., Conde-Gonzáles, J., and Perales, J. C. (2017). La fatiga como estado motivacional subjetivo. Rev. Andaluza Med. Deporte 10, 31–41. doi: 10.1016/j.ramd.2016.04.001
Clemente, V. (2016). Cortical arousal and central nervous system fatigue after a mountain marathon. Cult. Ciencia Deporte 12, 143–148. doi: 10.12800/ccd.v12i35.886
Clemente, V., De la Vega, R., Robles, J. J., Lautenschlaeger, M., and Fernández-Lucas, J. (2016). Experience modulates the psychophysiological response of airborne warfighters during a tactical combat parachute jump. Int. J. Psychophysiol. 110, 212–216. doi: 10.1016/j.ijpsycho.2016.07.502
Clemente, V., and Díaz, M. (2019). Evaluation of central fatigue by the critical flicker fusion threshold in cyclist. J. Med. Syst. 43:61. doi: 10.1007/s10916-019-1170-3
Clemente, V., Muñoz, V., and Melús, M. (2011). Fatiga del sistema nervio-so después de realizar un test de capacidad de sprints repetidos (RSA) en jugadores de futbol profesionales. Arch. Med. Deporte 143, 103–112.
Cohen, J. (1988). Statistical Power Analysis for the Behavioral Sciences , 2nd Edn. New York, NY: Academic Press.
Davranche, K., and Pichon, A. (2005). Critical flicker frequency threshold increment after an exhausting exercise. J. Sport Exerc. Psychol. 27:515. doi: 10.1123/jsep.27.4.515
Folkman, S., and Lazarus, R. S. (1988). Coping as a mediator of emotion. J. Pers. Soc. Psychol. 54, 466–475. doi: 10.1037/0022-3514.54.3.466
Fuentes, J. P., Villafaina, S., Collado, D., De la Vega, R., Olivares, P., and Clemente, V. (2019). Differences between high vs. low performance chess players in heart rate variability during chess problems. Front. Psychol. 10:409. doi: 10.3389/fpsyg.2019.00409
Gendolla, G. H. E., and Richter, M. (2010). Effort mobilization when the self is involved: some lessons from the cardiovascular system. Rev. Gen. Psychol. 14, 212–226. doi: 10.1037/a0019742
Gómez-Oliva, E., Robles-Pérez, J. J., Ruiz-Barquín, R., Hidalgo-Bellota, F., and de la Vega, R. (2019). Psychophysiological response to the use of nuclear, biological and chemical equipment with military tasks. Physiol. Behav. 204, 186–190. doi: 10.1016/j.physbeh.2019.02.019
Görtelmeyer, R., and Zimmermann, H. (1982). Retest reliability and construct validity of critical flicker fusion frequency. Pharmacopsychiatry 15, 24–28. doi: 10.1055/s-2007-1019545
Guggisberg, A., and Mottaz, A. (2013). Timing and awareness of movement decisions: does consciousness really come too late? Front. Hum. Neurosci. 7:385. doi: 10.3389/fnhum.2013.00385
Haider, M., Groll-Knapp, E., and Ganglberger, J. A. (1981). Event-related slow (DC) potentials in the human brain. Rev. Physiol. Biochem. Pharmacol. 88, 125–195. doi: 10.1007/BFb0034537
Harriss, D. J., Macsween, A., and Atkinson, G. (2019). Ethical standards in sport and exercise science research: 2020 update. Int. J. Sports Med. 40, 813–817. doi: 10.1055/a-1015-3123
Ilyukhina, V. A. (1986). Neirofiziologiya funktsional’nykh sostoyanii cheloveka (Neurophysiology of Human Functional States). Nauka: Leningrad.
Ilyukhina, V. A. (2015). Contributions of academicians A. A. Ukhtomsky and N. P. Bechtereva to multidisciplinary human brain science. Cogn. Syst. Monogr. 25, 81–100. doi: 10.1007/978-3-319-19446-2_5
Ilyukhina, V. (2013). Ultraslow information control systems in the integration of life activity processes in the brain and body. Hum. Physiol. 39, 323–333. doi: 10.1134/S0362119713030092
Ilyukhina, V., Sychev, A., Shcherbakova, N., Baryshev, G., and Denisova, V. (1982). The omegapotential: a quantitative parameter of the state of brain structures and of the individual: II. Possibilities and limitations of the use of the omega-potential for rapid assessment of the state of the individual. Hum. Physiol. 8, 328–339.
Ilyukhina, V. A., and Zabolotskikh, I. B. (1997). The typology of spontaneous and induced dynamics of superslow physiological processes recorded from the surface of the head and the body of a healthy and sick man. Kuban Sci. Med. Bull. 4:12.
Ilyukhina, V. A., and Zabolotskikh, I. B. (2020). Physiological basis of differences in the body tolerance to submaximal physical load to capacity in healthy young individuals. Hum. Physiol. 26, 330–336. doi: 10.1007/BF02760195
Inzlicht, M., and Marcora, S. M. (2016). The central governor model of exercise regulation teaches us precious little about the nature of mental fatigue and self-control failure. Front. Psychol. 7:656. doi: 10.3389/fpsyg.2016.00656
Lazarus, R. S. (1990). Theory-based stress measurement. Psychol. Inq. 1, 3–13. doi: 10.1207/s15327965pli0101_1
Li, Z., Jiao, K., Chen, M., and Wang, C. (2004). Reducing the effects of driving fatigue with magnitopuncture stimulation. Accident Anal. Prevent. 36, 501–505. doi: 10.1016/S0001-4575(03)00044-7
Lohani, M., Payne, B. R., and Strayer, D. L. (2019). A review of psychophysiological measures to assess cognitive states in real-world driving. Front. Hum. Neurosci. 19:57. doi: 10.3389/fnhum.2019.00057
Montero, I., and León, O. G. (2007). A guide for naming research studies in psychology. Int. J. Clin. Health Psychol. 7, 847–862.
Naranjo-Orellana, J., Ruso-Álvarez, J. F., and Rojo-Álvarez, J. L. (2020). Comparison of Omegawave device and an ambulatory ECG for RR interval measurement at rest. Int. J. Sport Med. [Epub ahead of print]. doi: 10.1055/a-1157-9220
Neuwirth, W., and Benesch, M. (2012). Vienna Test System Manual: Determination Test, (Version 35). Moedling: Schuhfried.
Noble, R. J., and Robertson, R. J. (1996). Perceived Exertion. Champaign, IL: Human Kinetics, 77–81.
Ong, N. C. H. (2015). The use of the Vienna Test System in sport psychology research: a review. Int. Rev. Sport Exerc. Psychol. 8, 204–223. doi: 10.1080/1750984X.2015.106158
Rösler, F., Heil, M., and Ridder, B. (1997). Slow negative brain potentials as reflections of specific modular resources of cognition. Biol. Psychol. 45, 109–141. doi: 10.1016/S0301-0511(96)05225-8
Schuhfried, G. (2013). Vienna Test System: Psychological Assessment. Moedling: Schuhfried.
Shields, G. S., Sazma, M. A., and Yonelinas, A. P. (2016). The effects of acute stress on core executive functions: a meta-analysis and comparison with cortisol. Neurosci. Biobehav. Rev. 68, 661–668. doi: 10.1016/j.neubiorev.2016.06.038
Tarvainen, M. P., Niskanen, J. P., Lipponen, J. A., Ranta-aho, P. O., and Karjalainen, P. A. (2014). Kubios HRV - Heart rate variability analysis software. Comput. Methods Progr. Biomed. 113, 210–220. doi: 10.1016/j.cmpb.2013.07.024
Tomczak, M., and Tomcak, E. (2014). The need to report effect size estimates revisited. An overwiew of some recommended measures of effect size. Trends Sport Sci. 1, 19–25.
Valenzuela, P. L., Sánchez-Martínez, G., Torrontegi, E., Vázquez-Carrión, J., Montalvo, Z., and Kara, O. (2020). Validity, reliability, and sensitivity to exercise-induced fatigue of a customer-friendly device for the measurement of the brain’s direct current potencial. J. Strength Condition. Res. [Epub ahead of print]. doi: 10.1519/JSC.0000000000003695
Vicente-Rodríguez, M., Fuentes-García, J. P., and Clemente-Suárez, V. J. (2020). Psychophysiological stress response in an underwater evacuation training. Int. J. Environ. Res. Public Health 17:2307. doi: 10.3390/ijerph17072307
Wagshul, M. E., Eide, P. K., and Madsen, J. R. (2011). The pulsating brain: a review of experimental and clinical studies of intracranial pulsatility. Fluids Barriers CNS 8, 1–23. doi: 10.1186/2045-8118-8-5
Whiteside, A. (2002). A synopsis of the vienna test system: a computer aided psychological diagnosis. J. Occup. Psychol. Employment Disabil. 5, 41–50.
Whiteside, A., Parker, G., and Snodgrass, R. (2003). A review of selected tests from the Vienna test system. Select. Dev. Rev. 19, 7–11.
Wijesuriya, N., Tran, Y., and Craig, A. (2007). The psychophysiological determinants of fatigue. Int. J. Psychophysiol. 63, 77–86. doi: 10.1016/j.ijppsycho.2006.08.005
Wilson, G. F., Caldwell, J. A., and Russell, C. A. (2007). Performance and psychophysiological measures of fatigue effects on aviation related tasks of varying difficulty. Int. J. Aviation Psychol. 17, 219–247. doi: 10.1080/10508410701328839
Woodworth, R. S., and Schlosberg, H. (1954). Experimental Psychology. New York, NY: Holt.
Keywords : central fatigue, omega wave, cognitive response, psychophysiology, stress
Citation: de la Vega R, Jiménez-Castuera R and Leyton-Román M (2021) Impact of Weekly Physical Activity on Stress Response: An Experimental Study. Front. Psychol. 11:608217. doi: 10.3389/fpsyg.2020.608217
Received: 19 September 2020; Accepted: 04 December 2020; Published: 12 January 2021.
Reviewed by:
Copyright © 2021 de la Vega, Jiménez-Castuera and Leyton-Román. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY) . The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marta Leyton-Román, bWFydGEubGV5dG9uQHVyamMuZXM=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Articles in 2020
Eukaryotic clamp loaders and unloaders in the maintenance of genome stability
- Kyoo-young Lee
- Su Hyung Park

Comparison of thrombus, gut, and oral microbiomes in Korean patients with ST-elevation myocardial infarction: a case–control study
- Ju-Seung Kwun
- Si-Hyuck Kang
Melatonin prevents doxorubicin-induced cardiotoxicity through suppression of AMPKα2-dependent mitochondrial damage
- Goowon Yang
- Minhyeok Song

Distinct genomic profiles of gestational choriocarcinoma, a unique cancer of pregnant tissues
- Seung-Hyun Jung
- Youn Jin Choi
- Sug Hyung Lee

Spermidine attenuates bleomycin-induced lung fibrosis by inducing autophagy and inhibiting endoplasmic reticulum stress (ERS)-induced cell death in mice
- Ae Rin Baek
- Sung Woo Park

Transplantation of Wnt5a-modified NSCs promotes tissue repair and locomotor functional recovery after spinal cord injury
- Zhiming Peng

LSD1: more than demethylation of histone lysine residues
- Bruno Perillo
- Alfonso Tramontano
- Antimo Migliaccio

Histone acylation marks respond to metabolic perturbations and enable cellular adaptation
- Seokjae Park
- Eun-Jung Cho
Development of a miRNA-controlled dual-sensing system and its application for targeting miR-21 signaling in tumorigenesis
- Sung Soo Kim
- Jong Heon Kim

Interactions between tumor-derived proteins and Toll-like receptors
- Gun-Young Jang
- Yeong-Min Park

Calsequestrin: a well-known but curious protein in skeletal muscle
- Jin Seok Woo
- Seung Yeon Jeong
- Eun Hui Lee
Tumor-promoting macrophages prevail in malignant ascites of advanced gastric cancer
- Hye Hyeon Eum
- Minsuk Kwon
- Woong-Yang Park

Shaping of the 3D genome by the ATPase machine cohesin
Hepatocellular carcinoma: old friends and new tricks.
- Patrick Viatour
Interleukin-11 signaling underlies fibrosis, parenchymal dysfunction, and chronic inflammation of the airway
- Benjamin Ng
- Stuart A. Cook
- Sebastian Schafer

Nuciferine modulates the gut microbiota and prevents obesity in high-fat diet-fed rats
Stress and the dopaminergic reward system
- Ja-Hyun Baik
Advances in transcriptome analysis of human brain aging
- Seokjin Ham
- Seung-Jae V. Lee


Single-cell network biology for resolving cellular heterogeneity in human diseases
FGF401 and vinorelbine synergistically mediate antitumor activity and vascular normalization in FGF19-dependent hepatocellular carcinoma
- Aldo Prawira
- Diana Graus Porta
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List
Recent Updates in Experimental Research and Clinical Evaluation on Drugs for COVID-19 Treatment
Huiqiang dai, yunchuang xiong, jing-quan wang, lusheng lin, zhe-sheng chen.
- Author information
- Article notes
- Copyright and License information
Edited by: Stephen Rennard , University of Nebraska Medical Center, United States
Reviewed by: Ji-Ye Yin , Central South University, China
Hongtao Xiao , University of Electronic Science and Technology of China, China
Yitao Wang , University of Macau, China
*Correspondence: Zhe-Sheng Chen, [email protected] ; Lusheng Lin, [email protected]
These authors contribute equally to the work.
This article was submitted to Respiratory Pharmacology, a section of the journal Frontiers in Pharmacology
Received 2021 Jul 13; Accepted 2021 Oct 13; Collection date 2021.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
Since the outbreak of corona virus disease 2019 (COVID-19) in Wuhan (China) in December 2019, the epidemic has rapidly spread to many countries around the world, posing a huge threat to global public health. In response to the pandemic, a number of clinical studies have been initiated to evaluate the effect of various treatments against COVID-19, combining medical strategies and clinical trial data from around the globe. Herein, we summarize the clinical evaluation about the drugs mentioned in this review for COVID-19 treatment. This review discusses the recent data regarding the efficacy of various treatments in COVID-19 patients, to control and prevent the outbreak.
Keywords: corona virus disease 2019, corona virus disease 2019 treatment, severe acute respiratory syndrome corona virus 2 variants, antimicrobials, immunotherapy, traditional Chinese medicine
Introduction
The outbreak of corona virus disease 2019 (COVID-19), from Wuhan, Hubei Province, China, in December 2019, has now become the first global pandemic caused by the spread of coronavirus. On February 11, 2020, the World Health Organization (WHO) gave a name for the novel coronavirus as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the coronavirus disease of 2019 (COVID-19) caused by SARS-CoV-2 ( Bevova et al., 2020 ). Most recently, several predominate SARS-CoV-2 variants, including, but not limited to, B.1.1.7 (alpha) variant, B.1.351 (beta) variant, P.1 (gamma), and B.1.617.2 (delta) variant, were first detected in the United Kingdom, South Africa, Brazil, and India, and became a novel global concern ( Ong et al., 2021 ; Sanches et al., 2021 ). The SARS-CoV-2 variants have greater ability of virus infectivity and immune escape, suggesting that the SARS-CoV-2 variants may result in poor treatment efficacy and prognosis for COVID-19 patients. In the past few months, many research teams from around the world have been conducting in vitro and in vivo studies of the virus, seeking effective prevention and control measures to prevent its spread. China is relatively fast and effective in the control of epidemic. We are, therefore, able to comprehensively analyze common domestic treatment methods and combined domestic and foreign research to jointly explore effective treatment programs for COVID-19, to provide guidance for the second wave of the epidemic.
Many products including, but not limited to, traditional Chinese medicines (TCMs), antiviral drugs (e.g., chloroquine phosphate and alpha-interferon) ( Wang and Zhu, 2020 ), monoclonal antibodies (e.g., tozumab combined with adamumab) ( Sarkar et al., 2020 ), convalescence plasma, and mesenchymal stem cells (MSCs) ( Peng et al., 2020 ) have become the focus of our communication for COVID-19 treatment. The Chinese Clinical Trial Registry (ChiCTR) shows a large number of TCM-related drugs studied for the treatment and prevention of COVID-19 (e.g., Lianhuaqingwen capsule, Shuanghuanglian oral liquid, Xuebijing injection, etc.) ( Li H. et al., 2020 ), while Western drugs focus on antiviral drugs and immunotherapy (e.g., stem cell-based therapy, antibodies, etc.) ( Ni et al., 2020a ; Gulati et al., 2021 ). In the Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7), it mentioned several antiviral drugs such as chloroquine (CQ), alpha-interferon (IFN-α), lopinavir/ritonavir, and umifenovir, and also mentioned immunotherapy, such as tocilizumab ( Wei, 2020a ; Zhao et al., 2020a ; Wei, 2020b ). Notably, as the adage, “old drug, new trick,” most of the antiviral drugs used for COVID-19 treatment are existing compounds screened for potential use based on mechanistic similarities to other viruses.
Herein, we summarize the clinical evaluation for COVID-19 treatment about the drugs mentioned in this review. Figure 1 depicts the overview of the organization of this review. Furthermore, we discuss recent representative progresses and considerations in the treatment for COVID-19, especially antimicrobials (antivirals and antibiotics/antibacterial), immunotherapy, and TCMs.
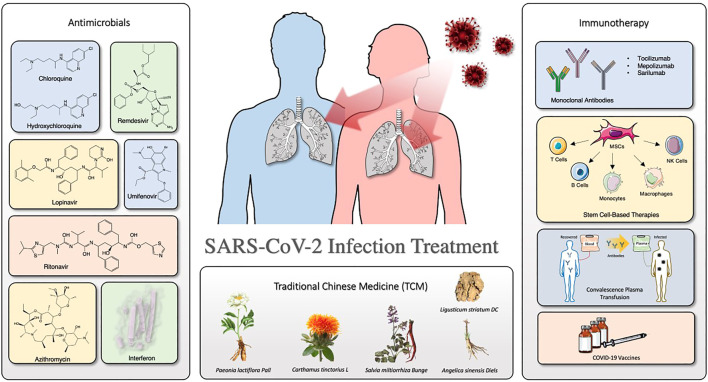
Overview of the organization of this review.
Antimicrobials
Chloroquine and hydroxychloroquine.
As a widely used antimalarial and immunomodulatory drug, chloroquine (CQ) shows a broad-spectrum antiviral activity. Table 1 summarizes the clinical trials of CQ and HCQ for the treatment of COVID-19. Some researchers indicated that CQ is effective against SARS-CoV-2 virus in early clinical studies ( Huang et al., 2020c ). Of note, chloroquine phosphate is undergoing some clinical trials regarding prophylactic use in health personnel (Clinicaltrials.gov, NCT04443270 ) and against infection by SARS-CoV-2 ( Clinicaltrials.gov , NCT04344951 ). Evidence from a multicenter prospective observational study indicated that patients in CQ treatment group have shorter median time to achieve an undetectable viral RNA and shorter duration of fever; also, more importantly, no severe side effects were found during CQ treatment ( Huang et al., 2020b ). Hydroxychloroquine (HCQ) is an analog of CQ by replacing an ethyl group in CQ with a hydroxyethyl group ( Zhou et al., 1878 ). Nowadays, ChiCTR conducts many clinical trials in China to examine the effectiveness and safety of CQ or HCQ against COVID-19 ( Gao et al., 2020 ). A team from Renmin Hospital of Wuhan University investigated the effects of HCQ among 62 patients suffering from COVID-19 ( www.chictr.org.cn , ChiCTR2000029559). As a result, Chen et al. found that HCQ could significantly shorten time to clinical recovery (TTCR) and improve pneumonia.
Summary of clinical trials of chloroquine (CQ) and hydroxychloroquine (HCQ) on COVID-19 treatment.
(All information in the table are collected from https://clinicaltrials.gov ).
However, the high-quality clinical data showing a clear and reliable benefit of CQ or HCQ remains limited. Also, the CQ or HCQ treatment could induce severe cardiac side effects, imped innate and adaptive antiviral immune responses, and cause some uncertain effects ( Meyerowitz et al., 2020 ). Commonly, QT prolongation and torsade de Pointes (TdP) occur on patients who are administered with CQ or HCQ ( Blignaut et al., 2019 ). Hence, before CQ and HCQ treatment, an initial cardiac evaluation is necessary for COVID-19 patients ( Zhou W. et al., 2020 ). Also, several follow-up evaluations, such as regular ophthalmological examination and cardiac monitor, are suggested for patients with short- or long-term treatment ( Knox and Owens, 1966 ). Thus, using CQ or HCQ as a COVID-19 treatment was controversial, which results from their ocular, cardiac, and neuro toxicities ( Oren et al., 2020 ; Zou et al., 2020 ). Additionally, the certainty of evidence is low. Together, we would like to recommend monitoring the accumulative effect of long-term and/or high-dose CQ or HCQ in clinical settings. Also, researchers are not supposed to overstate or understate the clinical efficacy of CQ and HCQ on COVID-19 treatment.
Lopinavir/ritonavir
Lopinavir/ritonavir tablets (brand name: Kaletra) are two structurally related protease inhibitors and works as antiretroviral agents ( Cvetkovic and Goa, 2003 ). Table 2 summarizes the clinical trials of lopinavir/ritonavir on COVID-19 treatment. The mechanism of action of protease inhibitors is block cleavage in Gag and Gag-Pol, and result in producing immature and noninfectious virus particles ( Adamson, 2012 ). Similar to CQ, lopinavir/ritonavir could act as potential antiviral agents against SARS in vitro and in patients with SARS infection ( Chu et al., 2004 ). Also, lopinavir/ritonavir has favorable clinical outcome with the Middle East respiratory syndrome coronavirus (MERS-CoV) after MERS reported in 2012 ( Mo and Fisher, 2016 ; Arabi et al., 2018 ). Evidence from randomized trials indicated that lopinavir/ritonavir might improve outcomes in severe and critical COVID-19 patients, but it may induce mortality ( Verdugo-Paiva et al., 2020 ). Moreover, it is reported that lopinavir/ritonavir could only improve a minority of throat-swab nucleic acid results in hospitals ( Liu et al., 2020 ). Also, Cao et al. revealed that no beneficial response or clinical improvement was observed after treatment with lopinavir/ritonavir in a randomized, controlled, open-label trial with 199 in hospital patients suffering from severe SARS-CoV-2 infection, even though improvement was found for some secondary endpoints ( Cao et al., 2020 ; Stower, 2020 ). Together, the response of COVID-19 patients with lopinavir/ritonavir is not ideal and unfavorable. As the previous study showed, CQ had more potent effects to patients with COVID-19 than the use of lopinavir/ritonavir; hence, an ongoing clinical trial in China would like to access the effectiveness and safety of CQ and lopinavir/ritonavir for patients suffering from mild or general SARS-CoV-2 infection ( www.chictr.org.cn , ChiCTR2000029741). Overall, available data on the anti-SARS-CoV-2 activity of lopinavir/ritonavir are still limited and investigational, thereby the clinical application of lopinavir/ritonavir should be considered and monitored carefully.
Summary of clinical trials of lopinavir/ritonavir on COVID-19 treatment.
Remdesivir (GS-5734, brand name: Veklury), as a nucleotide analog prodrug, is a broad-spectrum antiviral drug that acts on RNA-dependent RNA polymerase (RdRp) and results in premature termination ( Tchesnokov et al., 2019 ; Lamb, 2020 ). Table 3 shows the summary of clinical trials of remdesivir on COVID-19 treatment. As previously mentioned, Wang et al. showed that the EC 50 value of remdesivir is 1.76 μM in Vero E6 cells, which suggests that remdesivir has high effectiveness in the control of SARS-CoV-2 infection in vitro ( Wang M. et al., 2020 ). More importantly, the intravenous remdesivir was administrated to the patient who was the first case diagnosed as SARS-CoV-2 infection in the United States ( Holshue et al., 2020 ). No adverse effects were observed in association with the infusion; also, clinical benefits were found in patients. Another case demonstrated that remdesivir could accelerate recovery time by 4 days, which is a meaningful and optimistic progress for patients and medical systems ( Jorgensen et al., 2020 ). Notably, remdesivir is FDA approved specifically for the treatment of COVID-19. However, as more and more clinical cases were reported, the outcome of remdesivir treatment sometimes cannot achieve the expected effects on COVID-19 patients. Many researchers ( Wang Y. et al., 2020 ) carried out a randomized, double-blind, placebo-controlled, multicenter trial; as a result, Wang et al. found that remdesivir is not associated with statistically significant clinical improvement, even though some patients in the remdesivir treatment group had numerically faster time to improve than those in the placebo group. More importantly, remdesivir treatment was discontinued early due to the adverse events, including, but not limited to, nausea, constipation, and respiratory failure or acute respiratory distress. Overall, the certainty of evidence remains less. Since Nov. 2020, the WHO has issued a conditional recommendation against the use of remdesivir in COVID-19 patients.
Summary of clinical trials of remdesivir on COVID-19 treatment.
Interferons
The interferons (IFNs) as glycoproteins have broad-spectrum antiviral effects ( Lin and Young, 2014 ). The IFNs can be divided into three types based on the differences in the structures of their respective receptors. In detail, the IFNs are classified into type I IFNs (IFN-α/β), type II IFNs (IFN-γ), and type III IFNs (IFN-λ). Table 4 shows the summary of clinical trials of IFNs on COVID-19 treatment. Mantlo et al. (2020 ) demonstrated that IFN-α (EC 50 = 1.35 IU/ml) and IFN-β (EC 50 = 0.76 IU/ml) at clinically achievable concentrations could suppress the replication of SARC-CoV-2 in Vero cells. These findings provide a valuable fundamental for the potential use of IFN-α/β to against COVID-19. Zhou et al. accessed the efficacy of IFN-α2b and arbidol involving 77 hospitalized patients; as a result, researchers revealed that IFN-α2b with or without arbidol could significantly reduce the duration for detectable virus as well as the inflammatory markers ( Zhou Q. et al., 2020 ). Usually, the IFNs are used in combination with other antiviral therapies ( Mantlo et al., 2020 ). Of note, a group from China examined the effectiveness and safety profile of a triple antiviral therapy including IFN-β1b, lopinavir/ritonavir, and ribavirin with 86 patients suffering from mild to moderate SARS-CoV-2 infection ( Hung et al., 2020 ). Their results showed that the triple combination treatment is superior to lopinavir/ritonavir treatment alone with shorter viral shedding duration and hospital stay period.
Summary of clinical trials of interferons (IFNs) on COVID-19 treatment.
However, some reports indicated that the application of IFN-λ have more advantages in COVID-19 treatment. The most outstanding profile of IFN-λ over IFN-α/β is the absence of pro-inflammatory effects ( Prokunina-Olsson et al., 2020 ). This is because the response to IFN-λ administration localizes to epithelial cells, which could reduce side effects and inflammatory effects related to the systemic action from IFN-α/β treatment. Also, researchers showed that IFN-λ reduces the presence of virus in the lungs and prevents the induction of cytokine storm; hence, the application of IFN-λ could avoid pneumonia and acute respiratory distress syndrome (ARDS) ( Andreakos and Tsiodras, 2020 ). Overall, IFN-λ is a promising and potential therapeutic agent for patients suffering from COVID-19. Notably, more clinical study is necessary in the future.
Umifenovir (brand name: Arbidol, ARB) is an antiviral drug, which has the ability to inhibit the replication of influenza A and B virus through impeding the early membrane fusion event ( Leneva et al., 2009 ). Table 5 indicates the summary of clinical trials of umifenovir for the treatment of COVID-19. Zhu et al. (2020 ) accessed the efficacy and safety of lopinavir/ritonavir and umifenovir involving 50 COVID-19 patients, 34 cases with lopinavir/ritonavir treatment, and 16 cases with umifenovir treatment. From the results, no side effects and developed pneumonia or ARDS were observed in both groups. More importantly, patients with umifenovir treatment have shorter duration of positive RNA test compared with those with lopinavir/ritonavir treatment; thus, the authors indicated that umifenovir may be superior to lopinavir/ritonavir against COVID-19. Similarly, Deng et al. (2020 ) demonstrated that lopinavir/ritonavir combined with umifenovir had more favorable clinical outcomes compared with lopinavir/ritonavir only in a retrospective cohort study. Furthermore, Nojomi et al. (2020 ) evaluated HCQ followed by lopinavir/ritonavir or HCQ followed by umifenovir among 100 patients with COVID-19. As a result, the researchers found that patients in the umifenovir group had shorter hospitalized duration and higher peripheral oxygen saturation rate, also had improvements in requiring ICU admissions, and chest CT involvement. Moreover, some studies showed that umifenovir was well-tolerated with mild gastrointestinal tract reaction and related to the lower mortality in COVID-19 cases ( Jomah et al., 2020 ).
Summary of clinical trials of umifenovir on COVID-19 treatment.
However, Lian et al. (2020 ) indicated that umifenovir is not relative to the improved response in non-ICU COVID-19 patients in a retrospective study. In detail, the study included 81 patients suffering from COVID-19, and evaluated several baseline clinical and laboratory factors. Of note, the patients with umifenovir treatment even had longer hospital stay duration than those patients in the control group. Hence, the authors indicated that umifenovir might not improve prognosis or accelerate SARS-CoV-2 clearance in non-ICU patients with COVID-19.
Azithromycin
Azithromycin is a macrolide antibiotic medication. Azithromycin binds to the 50S subunit of ribosome, and thereby prevents the mRNA translation and interferes with protein synthesis ( Bakheit et al., 2014 ). Table 6 summarizes the clinical trials of azithromycin on COVID-19 treatment. Gautret et al. (2020 ) showed that azithromycin could reinforce the effectiveness of HCQ to clear the COVID-19 virus. Of note, the sample size was small, which only involved 20 cases. Also, researchers revealed that azithromycin combined with HCQ, or with lopinavir/ritonavir, could improve the clinical response and accelerate the COVID-19 virus clearance ( Purwati et al., 2021 ). By contrast, Cavalcanti et al. (2020 ) reported that no improved clinical outcomes were observed in COVID-19 patients, suffering from mild to moderate COVID-19, treated with HCQ alone or with azithromycin compared with those with standard care in a multicenter, randomized, open-label, three-group, controlled trial involving 667 patients. Also, evidence from retrospective observational studies demonstrated that azithromycin in combination with HCQ did not induce favorable clinical outcomes for COVID-19 patients ( Echeverría-Esnal et al., 2021 ).
Summary of clinical trials of azithromycin on COVID-19 treatment.
Antibacterial/antibiotic drugs
It has been reported that bacterial coinfection happened in 3.5% of COVID-19 patients ( Sieswerda et al., 2021 ). In other words, the hospitalized patients with COVID-19 have risk of bacterial infections. Sieswerda et al. (2021 ) recommended that the 5-day antibiotic therapy is required for the COVID-19 patients suffering with suspected bacterial respiratory infection after clinical improvements. However, their recommendation needs to be confirmed because unnecessary antibiotic treatment should be prevented. Also, some studies revealed that bacterial and fungal coinfection would occur in patients with SARS-CoV-2 infection, thereby the antimicrobial treatment regimen and stewardship interventions are necessary to control the exacerbating COVID-19 pandemic ( Rawson et al., 2020 ). More importantly, antimicrobial resistance should be considered as the collateral effect of SARS-CoV-2 infection, and thus, proper trend for antibiotic stewardship interventions should be analyzed and prescribed in the emergency department ( Pulia et al., 2020 ).
Immunotherapy
Monoclonal antibody, tocilizumab.
Tocilizumab (TCZ, trade name: Actemra) is a recombinant humanized monoclonal antibody ( Sheppard et al., 2017 ). TCZ is well-tolerated without significant abnormalities after long-term toxicity tests on animals ( Gabay et al., 2013 ). For the mechanism of action, TCZ specially binds membrane-bound interleukin-6 receptor (mIL-6R) and soluble interleukin-6 receptor (sIL-6R) and inhibits signal transduction ( Ibrahim et al., 2020 ). It has been reported that COVID-19 induces higher plasma levels of cytokines including, but not limited to, IL-6, IL-2, IL-7, IL-10, tumor necrosis factor-α (TNF-α), IFN-γ-inducible protein, etc., in ICU patients with SARS-CoV-2 infection ( Chen N. et al., 2020 ; Huang C. et al., 2020 ), which refers to a cytokine storm in patients. Furthermore, several studies indicated that TCZ treatment could return the temperature to normal quickly and improve the respiratory function through blocking IL-6 receptors ( Fu et al., 2020 ; Zhang et al., 2020 ). Table 7 shows the clinical trials of TCZ on COVID-19 treatment. Luo et al. (2020 ) examined the efficacy of TCZ, as a recombinant humanized antihuman IL-6 receptor monoclonal antibody, and found that the serum IL-6 level decreased in 10 patients, while the persistent and dramatic increase in IL-6 was found in four patients who failed in the treatment. In contrast, Xu et al. (2020 ) recorded the clinical manifestation, computerized tomography (CT) scan image, and laboratory examinations to assess the effectiveness of TCZ in severe COVID-19 patients. Their results showed that TCZ has critical roles in pathogenesis and clinical improvement in patients. Moreover, Klopfenstein et al. (2020 ) performed a retrospective case-control study involving 20 patients with severe SARS-CoV-2 infection and found that TCZ could reduce the number of ICU admissions and/or mortality compared with the patients without TCZ therapy. It should be noticed that the study performed by Klopfenstein et al. has some limitations, such as the small sample size and the retrospective nature of their work.
Summary of clinical trials of tocilizumab (TCZ) on COVID-19 treatment.
Interestingly, Stone et al. (2020 ) conducted a randomized, double-blind, placebo-controlled study (ClinicalTrials.gov, NCT04356937 ) with a larger sample size (243 patients with severe SARS-CoV-2 infection). The results from the study of Stone et al. demonstrated that TCZ is not effective in preventing intubation or death. However, some benefits, such as fewer serious infections in patients receiving TCZ therapy, cannot be ignored. Most recently, Salama et al. (2021 ) performed a trial enrolled with 389 COVID-19 patients (ClinicalTrials.gov, NCT04372186 ). The results showed that TCZ cannot improve survival rate; it only reduced the possibility of progression to the composite outcome of mechanical ventilation or death for the patients who were not receiving mechanical ventilation. Currently, TCZ undergoes several phase III clinical trials (Clinicaltrials.gov, NCT04423042 , NCT04356937 , NCT04403685 , etc.) to further understand the TCZ treatment as a supportive care option in alleviating the severe respiratory symptoms correlated with SARS-CoV-2 infection ( Alzghari and Acuña, 2020 ). Overall, TCZ appears to be an effective treatment for COVID-19 patients to calm the inflammatory storm and to reduce mortality. Notably, the efficacy of TCZ is controversial and remains to be further determined.
Mepolizumab
Mepolizumab (brand name: Nucala) is a human monoclonal antibody medication used for the treatment of severe eosinophilic asthma, eosinophilic granulomatosis, and hypereosinophilic syndrome (HES) ( Mukherjee et al., 2014 ; Ennis et al., 2019 ). Mepolizumab binds to IL-5 and prevents it from binding to its receptor on the surface of eosinophil white blood cells. Notably, some experts recommended to continue the mepolizumab therapy in COVID-19 patients with severe eosinophilic asthma, but the concern is that eosinopenia, which may serve as a diagnostic indicator for COVID-19 disease, may be a risk factor for worse disease outcomes ( Li Q. et al., 2020 ; Du et al., 2020 ; Bousquet et al., 2021 ). In other words, it is a challenge to manage patients with severe eosinophilic asthma infected by SARS-CoV-2. Aksu et al. (2021 ) reported that no evidence of loss of asthma control was observed during mepolizumab therapy in a woman patient with asthma infected by SARS-CoV-2. In addition, Azim et al. (2021 ) observed the outcomes from four patients receiving mepolizumab treatment. The researchers found that all four patients had a further reduction in their eosinophil counts within the reference range at the presentation with SARS-CoV-2 infection, but the underlying mechanism is not fully investigated, and subsequently recovered without any immediate evidence of long-term respiratory outcomes. Of note, one of four patients required hospitalization and ventilatory support. They thereby suggested that the mepolizumab therapy should be continued without any changed outcomes in the COVID-19 course. However, evidence from Eger et al. (2020 ) involved 634 severe asthma patients diagnosed with COVID-19 showed that patients with severe asthma receiving mepolizumab therapy have a more severe course of COVID-19 and an increasing risk of severity of COVID-19 compared with the general population. Overall, because the relevant data are limited, and the guideline is currently absent, maintaining or postponing mepolizumab treatment until the patient recovers from SARS-CoV-2 infection should be a case-by-case based decision for COVID-19 patients with severe asthma.
Sarilumab (brand name: Kevzara) is a humanized monoclonal antibody against IL-6 receptor. In 2017, FDA approved sarilumab for rheumatoid arthritis treatment ( Khiali et al., 2021 ). It has reported that severe COVID-19 disease is characterized by elevated serum levels of C reactive protein (CRP) and cytokines, including, but not limited to, IFN-γ, IL-8, and IL-6 ( Conti et al., 2020 ; Mo et al., 2020 ; Qin et al., 2020 ). Hence, this result provides a clue that anti-IL-6 agents have the possibility against SARS-CoV-2 infection. In a retrospective case report involving 15 COVID-19 patients, early intervention with sarilumab could have clinical improvement with decreased CRP level to patients with COVID-19 disease. More importantly, serum levels of CRP could be a potential biomarker for treatment response ( Montesarchio et al., 2020 ). An open-label cohort study assessed the clinical outcome of sarilumab among 28 patients infected by SARS-CoV-2 compared with 28 contemporary patients receiving standard of care alone ( Della-Torre et al., 2020 ). The results indicated that no significant difference was observed between sarilumab and standard of care. Of note, the clinical improvement suggested that sarilumab is relative to faster recovery in a subset of patients showing minor lung consolidation at baseline. In addition, there are several ongoing clinical trials to evaluate the effectiveness of sarilumab either plus standard of care ( Caballero Bermejo et al., 2020 ) or combined with corticosteroids (ClinicalTrials.gov, NCT04357808 ) ( Garcia-Vicuña et al., 2020 ) on COVID-19 disease. To date, the overall evaluation toward sarilumab on COVID-19 disease is much positive, which needs further tracking in the future.
Stem cell-based therapy
To date, most studies regarding stem-based therapy to SARS-CoV-2 infection have focused on mesenchymal stem cells (MSCs) ( Choudhery and Harris, 2020 ). MSC-based therapy has the ability to suppress the cytokine storm by secreting anti-inflammatory, anti-apoptosis, and antifibrosis cytokines. Also, MSCs contribute to antibacterial activity, as well as tissue repair and regeneration ( Sadeghi et al., 2020 ). Table 8 shows clinical trials of MSCs on COVID-19 treatment. For patients suffering from COVID-19, MSCs would repair damaged alveolar epithelial cells and blood vessels, and also prevent pulmonary fibrosis ( Chen et al., 2018 ; Leeman et al., 2019 ; Zanoni et al., 2019 ; Afra and Matin, 2020 ; Li Z. et al., 2020 ; Golchin et al., 2020 ). Seven COVID-19 patients who received intravenous transplantation of MSCs had significantly improved pulmonary function in 2 days after transplantation ( Leng et al., 2020 ). Notably, the increased peripheral lymphocytes and IL-10 level, decreased C-reactive protein (CRP) and TNF-α level, and disappeared overactivated cytokine-secreting immune cells were observed within 14 days after MSC injection. Interestingly, Jayaramayya et al. reported that MSC-derived exosomes (MSC-Exo) may be an option to improve the clinical response to COVID-19 patients ( Jayaramayya et al., 2020 ). A phase I clinical trial investigated the use of MSC-Exo inhalation to alleviate COVID-19-induced symptoms (clinicaltrials.gov, NCT04276987 ). Moreover, MSC-like derivatives have acceptable safety and efficacy for COVID-19 treatment in preclinical and clinical studies ( Li Z. et al., 2020 ).
Summary of clinical trials of mesenchymal stem cells (MSCs) on COVID-19 treatment.
However, some limitations remain to be considered ( Sadeghi et al., 2020 ). First, some patients with, including, but not limited to, a history of malignant tumor, coinfections of other respiratory viruses, and pregnant woman are not eligible to evolve in clinical trials. Most clinical trials worldwide remain in phase I and II, and comprehensive results are not clear. Furthermore, it is difficult to evaluate the effectiveness of MSC therapy alone when coadministration with other conventional drugs, such as remdesivir or dexamethasone, in many cases. Importantly, the standard therapeutic protocol, such as administration route, dosage, and transplantation frequency, needs to be determined. Nevertheless, the MSC profile on the immune system provides researchers evidence that it may be a good candidate as a combination therapy of infectious diseases such as COVID-19. Overall, MSC-based therapy appears to be a potential and promising therapeutic method to overcome SARS-CoV-2 infection.
Convalescence plasma transfusion
Convalescent plasma treatment provides immediate immunity by passive polyclonal antibody administration ( Mair-Jenkins et al., 2015 ). The efficacy of convalescent plasma transfusion may result from viremia suppression ( Chen L. et al., 2020 ). It has reported that convalescent plasma treatment can be used to improve the survival rate on patients with severe acute respiratory syndromes of viral etiology ( Mair-Jenkins et al., 2015 ). Several studies indicated that SARS patients who were treated with convalescent plasma had a shorter hospital stay and lower mortality than those who were not treated with convalescent plasma ( Soo et al., 2004 ; Cheng et al., 2005 ; Lai, 2005 ). Table 9 shows the clinical trials of convalescent plasma transfusion on COVID-19 treatment. Based on the findings from recent studies, initiating treatment no later than 5 days may be the most appropriate ( Woelfel et al., 2020 ; Zhao et al., 2020b ). Tiberghien et al. (2020 ) recommend that convalescent plasma administration at the early phases of the disease in patients at high risk of deleterious evolution may reduce the frequency of patient deterioration and, thereby, COVID-19 mortality. Also, close monitoring is necessary to detect any unintended side effects. However, a randomized trial (clinicaltrials.gov, NCT04383535 ) evolved in 228 COVID-19 patients to evaluate the clinical status after convalescent plasma intervention was added to standard treatment ( Simonovich et al., 2021 ). Unfortunately, no significant differences were found in clinical outcomes or overall mortality between patients infused with convalescent plasma added to standard treatment and those who received standard treatment alone within 30 days. Similarly, an open-label, multicenter, randomized clinical trial ( www.chictr.org.cn , ChiCTR2000029757) was performed in seven medical centers with 103 COVID-19 patients ( Li L. et al., 2020 ). The results showed that convalescent plasma therapy in addition to standard treatment, compared with standard treatment alone, did not result in a significant improvement in time to clinical improvement within 28 days. Of note, it is known that other treatments, including antiviral drugs, steroids, and intravenous immunoglobulin, have the possibility to affect the relationship between convalescent plasma and antibody level ( Luke et al., 2006 ). Thus, it is controversial whether it is worthwhile to examine the safety and efficacy of convalescent plasma intervention against SARS-CoV-2 infection in further randomized clinical trials.
Summary of clinical trials of convalescence plasma on COVID-19 treatment.
An efficacious vaccine is critical to prevent morbidity and mortality caused by COVID-19. There are four categories of COVID-19 vaccines under clinical evaluation, including whole-pathogen vaccines (inactivated vaccines), subunit vaccines, and nucleic acid (DNA and mRNA) vaccines. However, defining and assessing an efficacious vaccine is complex. In the case of SARS-CoV-2 infection, an efficacious vaccine could reduce the likelihood of an infection in an individual, severity of a disease in an individual, or the degree of transmission within a population ( Hodgson et al., 2021 ). The comprehensive understanding of SARS-Cov-2 is unclear and evolving, thereby the outcomes for a COVID-19 vaccine are critically appraised with scientific rigor to understand their generalizability and clinical significance.
Currently, three vaccines are authorized in the United States: Pfizer-BioNTech (Name: BNT162b2), Moderna (Name: mRNA-1273), and Johnson and Johnson/Janssen (Name: JNJ-78436735). Tables 10 – 12 summarize the clinical trials of these vaccines for the treatment of COVID-19. Of note, people under 12 years old are not eligible to receive vaccine produced by Pfizer-BioNTech, and people under 18 years old are not eligible to receive vaccines produced by Moderna and Johnson and Johnson/Janssen. Kamidani et al. (2021 ) indicated that children are supposed to have the opportunity to be included in clinical trials in parallel to ongoing adult phase III clinical trials. It is because the development of a pediatric COVID-19 vaccine could prevent disease and alleviate downstream effects including social isolation and interruption in education, thereby enabling children to re-engage in their world. Considering the SARS-CoV-2 variants, evidence from Polack et al. (2020 ) proved that BNT162b2 is 95% effective against SARS-CoV-2 infection. A 6 months of follow-up evaluation from Thomas et al. (2021 ) indicated that BNT162b2 has a favorable safety profile and effectively prevents COVID-19 for up to 6 months including the beta variant even though there is a gradual decline in effectiveness. Bernal et al. ( Lopez Bernal et al., 2021 ) reported that the efficacy of the one-shot BNT162b2 vaccine is 30.7% among individuals with the delta variant, while the efficacy is 48.7% among individuals with the alpha variant. The efficacy of two shots of BNT162b2 vaccine is 88.0% among individuals with the delta variant, while the efficacy is 93.7% among individuals with the alpha variant. In other words, as CDC recommendation, vaccination against COVID-19 is the best way to stop the spread of these predominate COVID-19 strains.
Summary of clinical trials of BNT162b2 vaccine (produced by Pfizer-BioNTech) on COVID-19 treatment.
Summary of clinical trials of JNJ-78436735 vaccine (produced by Johnson and Johnson/Janssen) on COVID-19 treatment.
Summary of clinical trials of mRNA-1273 vaccine (produced by Moderna) on COVID-19 treatment.
Most recently, a COVID-19 vaccine booster emerged to help individuals build enough protection after vaccination. According to the information from Centers for Disease Control and Prevention (CDC, https://www.cdc.gov ), individuals who have received their second dose of an mRNA COVID-19 vaccine (produced by either Pfizer-BioNTech or Moderna) for 8 months are eligible to get a booster shot. Currently, for individuals who got Johnson and Johnson/Janssen vaccine, there is not enough data to support getting an mRNA vaccine dose.
Traditional Chinese medicine
Xuebijing injection (XBJ) consists of Carthamus tinctorius L., Paeonia lactiflora Pall., Ligusticum striatum DC., Salvia miltiorrhiza Bunge, and Angelica sinensis (Oliv.) Diels ( Shi et al., 2017 ). XBJ constructs a “drug-ingredient-target-pathway” effector network to exert its therapeutic effects on COVID-19 prevention and treatment ( Zheng et al., 2020 ). Guo et al. (2020 ) conducted a retrospective case-control study to determine the efficacy of XBJ on SARS-CoV-2 infection with 42 patients who received routine treatment combined with XBJ (observation group) and 16 patients who received routine treatment alone (control group). The results showed that patients in the observation group had a significant reduction in body temperature, improvement in CT imaging results, and shorter time in a negative nucleic acid test recovery relative to those in the control group. Also, improvement in IL-6 levels was found in the observation group compared with those in the control group, while TNF-α and IL-10 levels did not show significant differences between the two groups. In addition, 284 COVID-19 patients were enrolled in a multicenter, prospective, randomized controlled trial to assess the effectiveness of Lianhuaqingwen (LH) capsule ( Hu et al., 2021 ). Compared with patients in the control group (received usual treatment alone), patients with usual treatment in combination with LH capsule treatment had higher recovery rate, shorter median time to symptom recovery, and higher rate of improvements in chest CT manifestations and clinical cure. Hence, both XBJ and LH capsules could be considered to ameliorate clinical symptoms of COVID-19. Moreover, Ni et al. reported that using Western medicine combined with Chinese traditional patent medicine Shuanghuanglian oral liquid (SHL) has expected therapeutic outcomes to COVID-19 patients, and thereby warrants further clinical trials ( Ni et al., 2020b ).
Concluding remarks
For antimicrobial drugs, the acquired drug resistance should be considered and explored. The use of CQ and HCQ is controversial due to their toxicity and side effects. Moreover, lopinavir/ritonavir, umifenovir, and azithromycin appear to be promising therapeutic drugs even though some studies do not show ideal and unfavorable clinical outcomes on COVID-19 patients. The IFNs are usually used in addition to other antiviral drugs. Also, the application of IFN-λ have more advantages than other types of IFNs in COVID-19 treatment.
TCZ, an antibody, has the ability to improve clinical responses on COVID-19 patients by suppressing inflammatory storm and, thereby, reduces mortality cases. Mepolizumab, as an antibody medication for asthma, may increase the risk of severe COVID-19 and induce a more severe course of COVID-19, particularly for COVID-19 patients with severe asthma receiving mepolizumab therapy. Sarilumab, as an FDA-approved antibody medication for rheumatoid arthritis treatment, shows clinical improvement with decreased CRP level to patients with COVID-19 disease. Furthermore, stem cell-based therapy, especially MSCs, could improve clinical symptoms and repair tissue caused by SARS-CoV-2 infection. Of note, the standard protocol of MSCs therapy needs to be determined. Additionally, COVID-19 patients who received convalescent plasma transfusion in addition to standard treatment shows no clinical differences compared with those who received standard treatment alone. Therefore, it is controversial whether it is worthwhile to assess the safety and efficacy of convalescent plasma intervention against SARS-CoV-2 infection in further randomized clinical trials.
In addition, TCMs play a critical role in ameliorating and alleviating clinical symptoms on COVID-19 patients. Also, it is known that TCMs in combination with Western medicine is a potential therapeutic strategy against SARS-CoV-2 infection.
To date, remdesivir is FDA approved specifically for the treatment of COVID-19. Also, several vaccines are authorized and recommended in the United States and other countries. Most treatment regimens against the COVID-19 pandemic are controversial and remain under preclinical and clinical trials. Overall, more comprehensive information regarding each treatment regimen is uncertain and needs to be further explored.
Acknowledgments
We thank Yangmin Chen (St. John’s University) for editing the article. Thanks to all the peer reviewers and editors for their opinions and suggestions.
Author Contributions
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
This work was partially supported by the Second Batch of Outstanding Young Medical Talents in Ganzhou City Health System (Jiangxi, China). The author (YY) thanks the support as a teaching fellow from Department of Pharmaceutical Sciences, St. John’s University (New York, United States).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
- Adamson C. S. (2012). Protease-Mediated Maturation of HIV: Inhibitors of Protease and the Maturation Process. Mol. Biol. Int. 2012, 604261. 10.1155/2012/604261 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Afra S., Matin M. M. (2020). Potential of Mesenchymal Stem Cells for Bioengineered Blood Vessels in Comparison with Other Eligible Cell Sources. Cell Tissue Res 380 (1), 1–13. 10.1007/s00441-019-03161-0 [ DOI ] [ PubMed ] [ Google Scholar ]
- Aksu K., Yesilkaya S., Topel M., Turkyilmaz S., Ercelebi D. C., Oncul A., et al. (2021). COVID-19 in a Patient with Severe Asthma Using Mepolizumab. Allergy Asthma Proc. 42 (2), e55–e57. 10.2500/aap.2021.42.200125 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Alzghari S. K., Acuña V. S. (2020). Supportive Treatment with Tocilizumab for COVID-19: A Systematic Review. J. Clin. Virol. 127, 104380. 10.1016/j.jcv.2020.104380 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Andreakos E., Tsiodras S. (2020). COVID-19: Lambda Interferon against Viral Load and Hyperinflammation. EMBO Mol. Med. 12 (6), e12465. 10.15252/emmm.202012465 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Arabi Y. M., Alothman A., Balkhy H. H., Al-Dawood A., AlJohani S., Al Harbi S., et al. (2018). Treatment of Middle East Respiratory Syndrome with a Combination of Lopinavir-Ritonavir and Interferon-Β1b (MIRACLE Trial): Study Protocol for a Randomized Controlled Trial. Trials 19 (1), 81. 10.1186/s13063-017-2427-0 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Azim A., Pini L., Khakwani Z., Kumar S., Howarth P. (2021). Severe Acute Respiratory Syndrome Coronavirus 2 Infection in Those on Mepolizumab Therapy. Ann. Allergy Asthma Immunol. 126 (4), 438–440. 10.1016/j.anai.2021.01.00610.1097/COH.0000000000000658 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Bakheit A. H., Al-Hadiya B. M., Abd-Elgalil A. A. (2014). Azithromycin. Profiles Drug Subst. Excip Relat. Methodol. 39, 1–40. 10.1016/b978-0-12-800173-8.00001-5 [ DOI ] [ PubMed ] [ Google Scholar ]
- Bevova M. R., Netesov S. V., Aulchenko Y. S. (2020). The New Coronavirus COVID-19 Infection. Mol. Gen. Microbiol. Virol. 35 (2), 53–60. 10.3103/s0891416820020044 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Blignaut M., Espach Y., van Vuuren M., Dhanabalan K., Huisamen B. (2019). Revisiting the Cardiotoxic Effect of Chloroquine. Cardiovasc. Drugs Ther. 33 (1), 1–11. 10.1007/s10557-018-06847-9 [ DOI ] [ PubMed ] [ Google Scholar ]
- Bousquet J., Jutel M., Akdis C. A., Klimek L., Pfaar O., Nadeau K. C., et al. (2021). ARIA-EAACI Statement on Asthma and COVID-19 (June 2, 2020). Allergy 76 (3), 689–697. 10.1111/all.14471 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Caballero Bermejo A. F., Ruiz-Antorán B., Fernández Cruz A., Diago Sempere E., Callejas Díaz A., Múñez Rubio E., et al. (2020). Sarilumab versus Standard of Care for the Early Treatment of COVID-19 Pneumonia in Hospitalized Patients: SARTRE: a Structured Summary of a Study Protocol for a Randomised Controlled Trial. Trials 21 (1), 794. 10.1186/s13063-020-04633-3 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cao B., Wang Y., Wen D., Liu W., Wang J., Fan G., et al. (2020). A Trial of Lopinavir-Ritonavir in Adults Hospitalized with Severe Covid-19. N. Engl. J. Med. 382 (19), 1787–1799. 10.1056/NEJMoa2001282 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cavalcanti A. B., Zampieri F. G., Rosa R. G., Azevedo L. C. P., Veiga V. C., Avezum A., et al. (2020). Hydroxychloroquine with or without Azithromycin in Mild-To-Moderate Covid-19. N. Engl. J. Med. 383 (21), 2041–2052. 10.1056/NEJMoa2019014 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chen L., Xiong J., Bao L., Shi Y. (2020a). Convalescent Plasma as a Potential Therapy for COVID-19. Lancet Infect. Dis. 20 (4), 398–400. 10.1016/s1473-3099(20)30141-9 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., et al. (2020b). Epidemiological and Clinical Characteristics of 99 Cases of 2019 Novel Coronavirus Pneumonia in Wuhan, China: a Descriptive Study. Lancet 395 (10223), 507–513. 10.1016/s0140-6736(20)30211-7 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chen S., Cui G., Peng C., Lavin M. F., Sun X., Zhang E., et al. (2018). Transplantation of Adipose-Derived Mesenchymal Stem Cells Attenuates Pulmonary Fibrosis of Silicosis via Anti-inflammatory and Anti-apoptosis Effects in Rats. Stem Cel Res Ther 9 (1), 110. 10.1186/s13287-018-0846-9 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Cheng Y., Wong R., Soo Y. O., Wong W. S., Lee C. K., Ng M. H., et al. (2005). Use of Convalescent Plasma Therapy in SARS Patients in Hong Kong. Eur. J. Clin. Microbiol. Infect. Dis. 24 (1), 44–46. 10.1007/s10096-004-1271-9 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Choudhery M. S., Harris D. T. (2020). Stem Cell Therapy for COVID-19: Possibilities and Challenges. Cell Biol Int 44 (11), 2182–2191. 10.1002/cbin.11440 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Chu C. M., Cheng V. C., Hung I. F., Wong M. M., Chan K. H., Chan K. S., et al. (2004). Role of Lopinavir/ritonavir in the Treatment of SARS: Initial Virological and Clinical Findings. Thorax 59 (3), 252–256. 10.1136/thorax.2003.012658 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Conti P., Ronconi G., Caraffa A., Gallenga C. E., Ross R., Frydas I., et al. (2020). Induction of Pro-inflammatory Cytokines (IL-1 and IL-6) and Lung Inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): Anti-inflammatory Strategies. J. Biol. Regul. Homeost Agents 34 (2), 327–331. 10.23812/conti-e [ DOI ] [ PubMed ] [ Google Scholar ]
- Cvetkovic R. S., Goa K. L. (2003). Lopinavir/ritonavir: a Review of its Use in the Management of HIV Infection. Drugs 63 (8), 769–802. 10.2165/00003495-200363080-00004 [ DOI ] [ PubMed ] [ Google Scholar ]
- Della-Torre E., Campochiaro C., Cavalli G., De Luca G., Napolitano A., La Marca S., et al. (2020). Interleukin-6 Blockade with Sarilumab in Severe COVID-19 Pneumonia with Systemic Hyperinflammation: an Open-Label Cohort Study. Ann. Rheum. Dis. 79 (10), 1277–1285. 10.1136/annrheumdis-2020-218122 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Deng L., Li C., Zeng Q., Liu X., Li X., Zhang H., et al. (2020). Arbidol Combined with LPV/r versus LPV/r Alone against Corona Virus Disease 2019: A Retrospective Cohort Study. J. Infect. 81 (1), e1–e5. 10.1016/j.jinf.2020.03.002 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Du Y., Tu L., Zhu P., Mu M., Wang R., Yang P., et al. (2020). Clinical Features of 85 Fatal Cases of COVID-19 from Wuhan. A Retrospective Observational Study. Am. J. Respir. Crit. Care Med. 201 (11), 1372–1379. 10.1164/rccm.202003-0543OC [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Echeverría-Esnal D., Martin-Ontiyuelo C., Navarrete-Rouco M. E., De-Antonio Cuscó M., Ferrández O., Horcajada J. P., et al. (2021). Azithromycin in the Treatment of COVID-19: a Review. Expert Rev. Anti Infect. Ther. 19 (2), 147–163. 10.1080/14787210.2020.1813024 [ DOI ] [ PubMed ] [ Google Scholar ]
- Eger K., Hashimoto S., Braunstahl G. J., Brinke A. T., Patberg K. W., Beukert A., et al. (2020). Poor Outcome of SARS-CoV-2 Infection in Patients with Severe Asthma on Biologic Therapy. Respir. Med. 177, 106287. 10.1016/j.rmed.2020.106287 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ennis D., Lee J. K., Pagnoux C. (2019). Mepolizumab for the Treatment of Eosinophilic Granulomatosis with Polyangiitis. Expert Opin. Biol. Ther. 19 (7), 617–630. 10.1080/14712598.2019.1623875 [ DOI ] [ PubMed ] [ Google Scholar ]
- Fu B., Xu X., Wei H. (2020). Why Tocilizumab Could Be an Effective Treatment for Severe COVID-19. J. Transl Med. 18 (1), 164. 10.1186/s12967-020-02339-3 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gabay C., Emery P., van Vollenhoven R., Dikranian A., Alten R., Pavelka K., et al. (2013). Tocilizumab Monotherapy versus Adalimumab Monotherapy for Treatment of Rheumatoid Arthritis (ADACTA): a Randomised, Double-Blind, Controlled Phase 4 Trial. Lancet 381 (9877), 1541–1550. 10.1016/s0140-6736(13)60250-0 [ DOI ] [ PubMed ] [ Google Scholar ]
- Gao J., Tian Z., Yang X. (2020). Breakthrough: Chloroquine Phosphate Has Shown Apparent Efficacy in Treatment of COVID-19 Associated Pneumonia in Clinical Studies. Biosci. Trends 14 (1), 72–73. 10.5582/bst.2020.01047 [ DOI ] [ PubMed ] [ Google Scholar ]
- Garcia-Vicuña R., Abad-Santos F., González-Alvaro I., Ramos-Lima F., Sanz J. S. (2020). Subcutaneous Sarilumab in Hospitalised Patients with Moderate-Severe COVID-19 Infection Compared to the Standard of Care (SARCOVID): a Structured Summary of a Study Protocol for a Randomised Controlled Trial. Trials 21 (1), 772. 10.1186/s13063-020-04588-5 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gautret P., Lagier J. C., Parola P., Hoang V. T., Meddeb L., Mailhe M., et al. (2020). Hydroxychloroquine and Azithromycin as a Treatment of COVID-19: Results of an Open-Label Non-randomized Clinical Trial. Int. J. Antimicrob. Agents 56 (1), 105949. 10.1016/j.ijantimicag.2020.105949 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Golchin A., Seyedjafari E., Ardeshirylajimi A. (2020). Mesenchymal Stem Cell Therapy for COVID-19: Present or Future. Stem Cel Rev Rep 16 (3), 427–433. 10.1007/s12015-020-09973-w [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Gulati S., Muddasani R., Gustavo Bergerot P., Pal S. K. (2021). Systemic Therapy and COVID19: Immunotherapy and Chemotherapy. Urol. Oncol. 39 (4), 213–220. 10.1016/j.urolonc.2020.12.022 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Guo H., Zheng J., Huang G., Xiang Y., Lang C., Li B., et al. (2020). Xuebijing Injection in the Treatment of COVID-19: a Retrospective Case-Control Study. Ann. Palliat. Med. 9 (5), 3235–3248. 10.21037/apm-20-1478 [ DOI ] [ PubMed ] [ Google Scholar ]
- Hodgson S. H., Mansatta K., Mallett G., Harris V., Emary K. R. W., Pollard A. J. (2021). What Defines an Efficacious COVID-19 Vaccine? A Review of the Challenges Assessing the Clinical Efficacy of Vaccines against SARS-CoV-2. Lancet Infect. Dis. 21 (2), e26–e35. 10.1016/s1473-3099(20)30773-8 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Holshue M. L., DeBolt C., Lindquist S., Lofy K. H., Wiesman J., Bruce H., et al. (2020). First Case of 2019 Novel Coronavirus in the United States. N. Engl. J. Med. 382 (10), 929–936. 10.1056/NEJMoa2001191 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hu K., Guan W. J., Bi Y., Zhang W., Li L., Zhang B., et al. (2021). Efficacy and Safety of Lianhuaqingwen Capsules, a Repurposed Chinese Herb, in Patients with Coronavirus Disease 2019: A Multicenter, Prospective, Randomized Controlled Trial. Phytomedicine 85, 153242. 10.1016/j.phymed.2020.153242 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., et al. (2020a). Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China. Lancet 395 (10223), 497–506. 10.1016/s0140-6736(20)30183-5 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Huang M., Li M., Xiao F., Pang P., Liang J., Tang T., et al. (2020b). Preliminary Evidence from a Multicenter Prospective Observational Study of the Safety and Efficacy of Chloroquine for the Treatment of COVID-19. Natl. Sci. Rev. 7 (9), 1428–1436. 10.1101/2020.04.26.20081059 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Huang M., Tang T., Pang P., Li M., Ma R., Lu J., et al. (2020c). Treating COVID-19 with Chloroquine. J. Mol. Cel Biol 12 (4), 322–325. 10.1093/jmcb/mjaa014 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Hung I. F., Lung K. C., Tso E. Y., Liu R., Chung T. W., Chu M. Y., et al. (2020). Triple Combination of Interferon Beta-1b, Lopinavir-Ritonavir, and Ribavirin in the Treatment of Patients Admitted to Hospital with COVID-19: an Open-Label, Randomised, Phase 2 Trial. Lancet 395 (10238), 1695–1704. 10.1016/s0140-6736(20)31042-4 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ibrahim Y. F., Moussa R. A., Bayoumi A. M. A., Ahmed A. F. (2020). Tocilizumab Attenuates Acute Lung and Kidney Injuries and Improves Survival in a Rat Model of Sepsis via Down-Regulation of NF-κB/JNK: a Possible Role of P-Glycoprotein. Inflammopharmacology 28 (1), 215–230. 10.1007/s10787-019-00628-y [ DOI ] [ PubMed ] [ Google Scholar ]
- Jayaramayya K., Mahalaxmi I., Subramaniam M. D., Raj N., Dayem A. A., Lim K. M., et al. (2020). Immunomodulatory Effect of Mesenchymal Stem Cells and Mesenchymal Stem-Cell-Derived Exosomes for COVID-19 Treatment. BMB Rep. 53 (8), 400–412. 10.5483/BMBRep.2020.53.8.121 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jomah S., Asdaq S. M. B., Al-Yamani M. J. (2020). Clinical Efficacy of Antivirals against Novel Coronavirus (COVID-19): A Review. J. Infect. Public Health 13 (9), 1187–1195. 10.1016/j.jiph.2020.07.013 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Jorgensen S. C. J., Kebriaei R., Dresser L. D. (2020). Remdesivir: Review of Pharmacology, Pre-clinical Data, and Emerging Clinical Experience for COVID-19. Pharmacotherapy 40 (7), 659–671. 10.1002/phar.2429 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Kamidani S., Rostad C. A., Anderson E. J. (2021). COVID-19 Vaccine Development: a Pediatric Perspective. Curr. Opin. Pediatr. 33 (1), 144–151. 10.1097/mop.0000000000000978 [ DOI ] [ PubMed ] [ Google Scholar ]
- Khiali S., Rezagholizadeh A., Entezari-Maleki T. (2021). A Comprehensive Review on Sarilumab in COVID-19. Expert Opin. Biol. Ther. 21 (5), 615–626. 10.1080/14712598.2021.1847269 [ DOI ] [ PubMed ] [ Google Scholar ]
- Klopfenstein T., Zayet S., Lohse A., Balblanc J. C., Badie J., Royer P. Y., et al. (2020). Tocilizumab Therapy Reduced Intensive Care Unit Admissions And/or Mortality in COVID-19 Patients. Med. Mal Infect. 50 (5), 397–400. 10.1016/j.medmal.2020.05.001 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Knox J. M., Owens D. W. (1966). The Chloroquine Mystery. Arch. Dermatol. 94 (2), 205–214. 10.1001/archderm.1966.01600260097016 [ DOI ] [ PubMed ] [ Google Scholar ]
- Lai S. T. (2005). Treatment of Severe Acute Respiratory Syndrome. Eur. J. Clin. Microbiol. Infect. Dis. 24 (9), 583–591. 10.1007/s10096-005-0004-z [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lamb Y. N. (2020). Remdesivir: First Approval. Drugs 80 (13), 1355–1363. 10.1007/s40265-020-01378-w [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Leeman K. T., Pessina P., Lee J. H., Kim C. F. (2019). Mesenchymal Stem Cells Increase Alveolar Differentiation in Lung Progenitor Organoid Cultures. Sci. Rep. 9 (1), 6479. 10.1038/s41598-019-42819-1 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Leneva I. A., Russell R. J., Boriskin Y. S., Hay A. J. (2009). Characteristics of Arbidol-Resistant Mutants of Influenza Virus: Implications for the Mechanism of Anti-influenza Action of Arbidol. Antivir. Res 81 (2), 132–140. 10.1016/j.antiviral.2008.10.009 [ DOI ] [ PubMed ] [ Google Scholar ]
- Leng Z., Zhu R., Hou W., Feng Y., Yang Y., Han Q., et al. (2020). Transplantation of ACE2(-) Mesenchymal Stem Cells Improves the Outcome of Patients with COVID-19 Pneumonia. Aging Dis. 11 (2), 216–228. 10.14336/ad.2020.0228 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Li H., Yang L., Liu F. F., Ma X. N., He P. L., Tang W., et al. (2020a). Overview of Therapeutic Drug Research for COVID-19 in China. Acta Pharmacol. Sin 41 (9), 1133–1140. 10.1038/s41401-020-0438-y [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Li L., Zhang W., Hu Y., Tong X., Zheng S., Yang J., et al. (2020b). Effect of Convalescent Plasma Therapy on Time to Clinical Improvement in Patients with Severe and Life-Threatening COVID-19: A Randomized Clinical Trial. Jama 324 (5), 460–470. 10.1001/jama.2020.10044 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Li Q., Ding X., Xia G., Chen H. G., Chen F., Geng Z., et al. (2020c). Eosinopenia and Elevated C-Reactive Protein Facilitate Triage of COVID-19 Patients in Fever Clinic: A Retrospective Case-Control Study. EClinicalMedicine 23, 100375. 10.1016/j.eclinm.2020.100375 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Li Z., Niu S., Guo B., Gao T., Wang L., Wang Y., et al. (2020d). Stem Cell Therapy for COVID-19, ARDS and Pulmonary Fibrosis. Cell Prolif 53 (12), e12939. 10.1111/cpr.12939 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lian N., Xie H., Lin S., Huang J., Zhao J., Lin Q. (2020). Umifenovir Treatment Is Not Associated with Improved Outcomes in Patients with Coronavirus Disease 2019: a Retrospective Study. Clin. Microbiol. Infect. 26 (7), 917–921. 10.1016/j.cmi.2020.04.026 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lin F. C., Young H. A. (2014). Interferons: Success in Anti-viral Immunotherapy. Cytokine Growth Factor. Rev. 25 (4), 369–376. 10.1016/j.cytogfr.2014.07.015 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Liu X., Chen H., Shang Y., Zhu H., Chen G., Chen Y., et al. (2020). Efficacy of Chloroquine versus Lopinavir/ritonavir in Mild/general COVID-19 Infection: a Prospective, Open-Label, Multicenter, Randomized Controlled Clinical Study. Trials 21 (1), 622. 10.1186/s13063-020-04478-w [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Lopez Bernal J., Andrews N., Gower C., Gallagher E., Simmons R., Thelwall S., et al. (2021). Effectiveness of Covid-19 Vaccines against the B.1.617.2 (Delta) Variant. N. Engl. J. Med. 385 (7), 585–594. 10.1056/NEJMoa2108891 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Luke T. C., Kilbane E. M., Jackson J. L., Hoffman S. L. (2006). Meta-analysis: Convalescent Blood Products for Spanish Influenza Pneumonia: a Future H5N1 Treatment. Ann. Intern. Med. 145 (8), 599–609. 10.7326/0003-4819-145-8-200610170-00139 [ DOI ] [ PubMed ] [ Google Scholar ]
- Luo P., Liu Y., Qiu L., Liu X., Liu D., Li J. (2020). Tocilizumab Treatment in COVID-19: A Single center Experience. J. Med. Virol. 92 (7), 814–818. 10.1002/jmv.25801 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mair-Jenkins J., Saavedra-Campos M., Baillie J. K., Cleary P., Khaw F. M., Lim W. S., et al. (2015). The Effectiveness of Convalescent Plasma and Hyperimmune Immunoglobulin for the Treatment of Severe Acute Respiratory Infections of Viral Etiology: a Systematic Review and Exploratory Meta-Analysis. J. Infect. Dis. 211 (1), 80–90. 10.1093/infdis/jiu396 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mantlo E., Bukreyeva N., Maruyama J., Paessler S., Huang C. (2020). Antiviral Activities of Type I Interferons to SARS-CoV-2 Infection. Antivir. Res 179, 104811. 10.1016/j.antiviral.2020.104811 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Meyerowitz E. A., Vannier A. G. L., Friesen M. G. N., Schoenfeld S., Gelfand J. A., Callahan M. V., et al. (2020). Rethinking the Role of Hydroxychloroquine in the Treatment of COVID-19. Faseb j 34 (5), 6027–6037. 10.1096/fj.202000919 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mo P., Xing Y., Xiao Y., Deng L., Zhao Q., Wang H., et al. (2020). Clinical Characteristics of Refractory COVID-19 Pneumonia in Wuhan, China. Clin. Infect. Dis.. 10.1093/cid/ciaa270 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mo Y., Fisher D. (2016). A Review of Treatment Modalities for Middle East Respiratory Syndrome. J. Antimicrob. Chemother. 71 (12), 3340–3350. 10.1093/jac/dkw338 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Montesarchio V., Parrela R., Iommelli C., Bianco A., Manzillo E., Fraganza F., et al. (2020). Outcomes and Biomarker Analyses Among Patients with COVID-19 Treated with Interleukin 6 (IL-6) Receptor Antagonist Sarilumab at a Single Institution in Italy. J. Immunother. Cancer 8 (2). 10.1136/jitc-2020-001089 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Mukherjee M., Sehmi R., Nair P. (2014). Anti-IL5 Therapy for Asthma and beyond. World Allergy Organ. J. 7 (1), 32. 10.1186/1939-4551-7-32 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ni L., Chen L., Huang X., Han C., Xu J., Zhang H., et al. (2020a). Combating COVID-19 with Integrated Traditional Chinese and Western Medicine in China. Acta Pharm. Sin B 10 (7), 1149–1162. 10.1016/j.apsb.2020.06.009 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ni L., Zhou L., Zhou M., Zhao J., Wang D. W. (2020b). Combination of Western Medicine and Chinese Traditional Patent Medicine in Treating a Family Case of COVID-19. Front. Med. 14 (2), 210–214. 10.1007/s11684-020-0757-x [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Nojomi M., Yassin Z., Keyvani H., Makiani M. J., Roham M., Laali A., et al. (2020). Effect of Arbidol (Umifenovir) on COVID-19: a Randomized Controlled Trial. BMC Infect. Dis. 20 (1), 954. 10.1186/s12879-020-05698-w [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Ong S. W. X., Chiew C. J., Ang L. W., Mak T. M., Cui L., Toh M., et al. (2021). Clinical and Virological Features of SARS-CoV-2 Variants of Concern: a Retrospective Cohort Study Comparing B.1.1.7 (Alpha), B.1.315 (Beta), and B.1.617.2 (Delta). Clin. Infect. Dis.. 10.1093/cid/ciab721 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Oren O., Yang E. H., Gluckman T. J., Michos E. D., Blumenthal R. S., Gersh B. J. (2020). Use of Chloroquine and Hydroxychloroquine in COVID-19 and Cardiovascular Implications: Understanding Safety Discrepancies to Improve Interpretation and Design of Clinical Trials. Circ. Arrhythm Electrophysiol. 13 (6), e008688. 10.1161/circep.120.008688 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Peng H., Gong T., Huang X., Sun X., Luo H., Wang W., et al. (2020). A Synergistic Role of Convalescent Plasma and Mesenchymal Stem Cells in the Treatment of Severely Ill COVID-19 Patients: a Clinical Case Report. Stem Cel Res. Ther. 11 (1), 291. 10.1186/s13287-020-01802-8 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Polack F. P., Thomas S. J., Kitchin N., Absalon J., Gurtman A., Lockhart S., et al. (2020). Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. N. Engl. J. Med. 383 (27), 2603–2615. 10.1056/NEJMoa2034577 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Prokunina-Olsson L., Alphonse N., Dickenson R. E., Durbin J. E., Glenn J. S., Hartmann R., et al. (2020). COVID-19 and Emerging Viral Infections: The Case for Interferon Lambda. J. Exp. Med. 217 (5). 10.1084/jem.20200653 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Pulia M. S., Wolf I., Schulz L. T., Pop-Vicas A., Schwei R. J., Lindenauer P. K. (2020). COVID-19: An Emerging Threat to Antibiotic Stewardship in the Emergency Department. West. J. Emerg. Med. 21 (5), 1283–1286. 10.5811/westjem.2020.7.48848 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Purwati Budiono., Rachman B. E., Miatmoko A., Lardo S., ,Purnama Y. S., Laely M., et al. (2021). A Randomized, Double-Blind, Multicenter Clinical Study Comparing the Efficacy and Safety of a Drug Combination of Lopinavir/Ritonavir-Azithromycin, Lopinavir/Ritonavir-Doxycycline, and Azithromycin-Hydroxychloroquine for Patients Diagnosed with Mild to Moderate COVID-19 Infections. Biochem. Res. Int. 2021, 6685921. 10.1155/2021/6685921 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Qin C., Zhou L., Hu Z., Zhang S., Yang S., Tao Y., et al. (2020). Dysregulation of Immune Response in Patients with Coronavirus 2019 (COVID-19) in Wuhan, China. 71(15) , 762–768. 10.1093/cid/ciaa248 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Rawson T. M., Moore L. S. P., Zhu N., Ranganathan N., Skolimowska K., Gilchrist M., et al. (2020). Bacterial and Fungal Coinfection in Individuals with Coronavirus: A Rapid Review to Support COVID-19 Antimicrobial Prescribing. Clin. Infect. Dis. 71 (9), 2459–2468. 10.1093/cid/ciaa530 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sadeghi S., Soudi S., Shafiee A., Hashemi S. M. (2020). Mesenchymal Stem Cell Therapies for COVID-19: Current Status and Mechanism of Action. Life Sci. 262, 118493. 10.1016/j.lfs.2020.118493 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Salama C., Han J., Yau L., Reiss W. G., Kramer B., Neidhart J. D., et al. (2021). Tocilizumab in Patients Hospitalized with Covid-19 Pneumonia. N. Engl. J. Med. 384 (1), 20–30. 10.1056/NEJMoa2030340 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sanches P. R. S., Charlie-Silva I., Braz H. L. B., Bittar C., Freitas Calmon M., Rahal P., et al. (2021). Recent Advances in SARS-CoV-2 Spike Protein and RBD Mutations Comparison between New Variants Alpha (B.1.1.7, United Kingdom), Beta (B.1.351, South Africa), Gamma (P.1, Brazil) and Delta (B.1.617.2, India). J. Virus. Erad 7 (3), 100054. 10.1016/j.jve.2021.100054 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sarkar C., Mondal M., Torequl Islam M., Martorell M., Docea A. O., Maroyi A., et al. (2020). Potential Therapeutic Options for COVID-19: Current Status, Challenges, and Future Perspectives. 11(1428)572870. doi: 10.3389/fphar.2020.572870 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Sheppard M., Laskou F., Stapleton P. P., Hadavi S., Dasgupta B. (2017). Tocilizumab (Actemra). Hum. Vaccin. Immunother. 13 (9), 1972–1988. 10.1080/21645515.2017.1316909 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Shi H., Hong Y., Qian J., Cai X., Chen S. (2017). Xuebijing in the Treatment of Patients with Sepsis. Am. J. Emerg. Med. 35 (2), 285–291. 10.1016/j.ajem.2016.11.007 [ DOI ] [ PubMed ] [ Google Scholar ]
- Sieswerda E., de Boer M. G. J., Bonten M. M. J., Boersma W. G., Jonkers R. E., Aleva R. M., et al. (2021). Recommendations for Antibacterial Therapy in Adults with COVID-19 - an Evidence Based Guideline. Clin. Microbiol. Infect. 27 (1), 61–66. 10.1016/j.cmi.2020.09.041 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Simonovich V. A., Burgos Pratx L. D., Scibona P., Beruto M. V., Vallone M. G., Vázquez C., et al. (2021). A Randomized Trial of Convalescent Plasma in Covid-19 Severe Pneumonia. N. Engl. J. Med. 384 (7), 619–629. 10.1056/NEJMoa2031304 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Soo Y. O., Cheng Y., Wong R., Hui D. S., Lee C. K., Tsang K. K., et al. (2004). Retrospective Comparison of Convalescent Plasma with Continuing High-Dose Methylprednisolone Treatment in SARS Patients. Clin. Microbiol. Infect. 10 (7), 676–678. 10.1111/j.1469-0691.2004.00956.x [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stone J. H., Frigault M. J., Serling-Boyd N. J., Fernandes A. D., Harvey L., Foulkes A. S., et al. (2020). Efficacy of Tocilizumab in Patients Hospitalized with Covid-19. N. Engl. J. Med. 383 (24), 2333–2344. 10.1056/NEJMoa2028836 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Stower H. (2020). Lopinavir–ritonavir in Severe COVID-19. Nat. Med. 26 (4), 465. 10.1038/s41591-020-0849-9 [ DOI ] [ PubMed ] [ Google Scholar ]
- Tchesnokov E. P., Feng J. Y., Porter D. P., Götte M. (2019). Mechanism of Inhibition of Ebola Virus RNA-dependent RNA Polymerase by Remdesivir. Viruses 11 (4). 10.3390/v11040326 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Thomas S. J., Moreira E. D., Jr., Kitchin N., Absalon J., Gurtman A., Lockhart S., et al. (2021). Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine through 6 Months. N. Engl. J. Med.. 10.1056/NEJMoa2110345 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Tiberghien P., de Lamballerie X., Morel P., Gallian P., Lacombe K., Yazdanpanah Y. (2020). Collecting and Evaluating Convalescent Plasma for COVID-19 Treatment: Why and How. Vox Sang 115 (6), 488–494. 10.1111/vox.12926 [ DOI ] [ PubMed ] [ Google Scholar ]
- Verdugo-Paiva F., Izcovich A., Ragusa M., Rada G. (2020). Lopinavir-ritonavir for COVID-19: A Living Systematic Review. Medwave 20 (6), e7967. 10.5867/medwave.2020.06.7966 [ DOI ] [ PubMed ] [ Google Scholar ]
- Wang M., Cao R., Zhang L., Yang X., Liu J., Xu M., et al. (2020a). Remdesivir and Chloroquine Effectively Inhibit the Recently Emerged Novel Coronavirus (2019-nCoV) In Vitro . Cell Res 30 (3), 269–271. 10.1038/s41422-020-0282-0 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wang Y., Zhang D., Du G., Du R., Zhao J., Jin Y., et al. (2020b). Remdesivir in Adults with Severe COVID-19: a Randomised, Double-Blind, Placebo-Controlled, Multicentre Trial. Lancet 395 (10236), 1569–1578. 10.1016/s0140-6736(20)31022-9 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wang Y., Zhu L.-Q. (2020). Pharmaceutical Care Recommendations for Antiviral Treatments in Children with Coronavirus Disease 2019. World J. Pediatr. : WJP 16 (3), 271–274. 10.1007/s12519-020-00353-5 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wei P-F. (2020a). Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7). Chin. Med. J. (Engl) 133 (9), 1087–1095. 10.1097/cm9.0000000000000819 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Wei P-F. (2020b). Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7). Chin. Med. J. (Engl) 133 (9), 1087–1095. 10.1097/cm9.0000000000000819 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Woelfel R., Corman V. M., Guggemos W., Seilmaier M., Zange S., Mueller M. A., et al. (2020). Clinical Presentation and Virological Assessment of Hospitalized Cases of Coronavirus Disease 2019 in a Travel-Associated Transmission Cluster. [ Google Scholar ]
- Xu X., Han M., Li T., Sun W., Wang D., Fu B., et al. (2020). Effective Treatment of Severe COVID-19 Patients with Tocilizumab. Proc. Natl. Acad. Sci. U S A. 117 (20), 10970–10975. 10.1073/pnas.2005615117 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zanoni M., Cortesi M., Zamagni A., Tesei A. (2019). The Role of Mesenchymal Stem Cells in Radiation-Induced Lung Fibrosis. Int. J. Mol. Sci. 20 (16). 10.3390/ijms20163876 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhang C., Wu Z., Li J. W., Zhao H., Wang G. Q. (2020). Cytokine Release Syndrome in Severe COVID-19: Interleukin-6 Receptor Antagonist Tocilizumab May Be the Key to Reduce Mortality. Int. J. Antimicrob. Agents 55 (5), 105954. 10.1016/j.ijantimicag.2020.105954 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhao J.-Y., Yan J.-Y., Qu J.-M. (2020a). Interpretations of “Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial Version 7)”. 133(11) , 1347–1349. doi: 10.1097/cm9.0000000000000866 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhao J., Yuan Q., Wang H., Liu W., Liao X., Su Y., et al. (2020b2019). Antibody Responses to SARS-CoV-2 in Patients with Novel Coronavirus. disease 71 (16), 2027–2034. 10.1093/cid/ciaa344 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zheng W. J., Yan Q., Ni Y. S., Zhan S. F., Yang L. L., Zhuang H. F., et al. (2020). Examining the Effector Mechanisms of Xuebijing Injection on COVID-19 Based on Network Pharmacology. BioData Min 13, 17. 10.1186/s13040-020-00227-6 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhou Q., Chen V., Shannon C. P., Wei X. S., Xiang X., Wang X., et al. (2020a). Interferon-α2b Treatment for COVID-19. Front. Immunol. 11, 1061. 10.3389/fimmu.2020.01061 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhou W., Wang H., Yang Y., Chen Z. S., Zou C., Zhang J. (1878). Chloroquine against Malaria, Cancers and Viral Diseases, 5832. (Electronic)). [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhou W., Wang H., Yang Y., Chen Z. S., Zou C., Zhang J. (2020b). Chloroquine against Malaria, Cancers and Viral Diseases. Drug Discov. Today 25 (11), 2012–2022. 10.1016/j.drudis.2020.09.010 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zhu Z., Lu Z., Xu T., Chen C., Yang G., Zha T., et al. (2020). Arbidol Monotherapy Is superior to Lopinavir/ritonavir in Treating COVID-19. J. Infect. 81 (1), e21–e23. 10.1016/j.jinf.2020.03.060 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- Zou L., Dai L., Zhang X., Zhang Z., Zhang Z. (2020). Hydroxychloroquine and Chloroquine: a Potential and Controversial Treatment for COVID-19. Arch. Pharm. Res. 43 (8), 765–772. 10.1007/s12272-020-01258-7 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (1.2 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
This paper is in the following e-collection/theme issue:
Published on 24.11.2020 in Vol 22 , No 11 (2020) : November
Psychosocial Effects of the COVID-19 Pandemic: Large-scale Quasi-Experimental Study on Social Media
Authors of this article:

Original Paper
- Koustuv Saha 1 , BTech ;
- John Torous 2 , MD ;
- Eric D Caine 3 , MD ;
- Munmun De Choudhury 1 , PhD
1 School of Interactive Computing, Georgia Institute of Technology, Atlanta, GA, United States
2 Division of Digital Psychiatry, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA, United States
3 Department of Psychiatry, University of Rochester, Rochester, NY, United States
Corresponding Author:
Koustuv Saha, BTech
School of Interactive Computing
Georgia Institute of Technology
North Ave NW
Atlanta, GA, 30332
United States
Phone: 1 4046929496
Email: [email protected]
Background: The COVID-19 pandemic has caused several disruptions in personal and collective lives worldwide. The uncertainties surrounding the pandemic have also led to multifaceted mental health concerns, which can be exacerbated with precautionary measures such as social distancing and self-quarantining, as well as societal impacts such as economic downturn and job loss. Despite noting this as a “mental health tsunami”, the psychological effects of the COVID-19 crisis remain unexplored at scale. Consequently, public health stakeholders are currently limited in identifying ways to provide timely and tailored support during these circumstances.
Objective: Our study aims to provide insights regarding people’s psychosocial concerns during the COVID-19 pandemic by leveraging social media data. We aim to study the temporal and linguistic changes in symptomatic mental health and support expressions in the pandemic context.
Methods: We obtained about 60 million Twitter streaming posts originating from the United States from March 24 to May 24, 2020, and compared these with about 40 million posts from a comparable period in 2019 to attribute the effect of COVID-19 on people’s social media self-disclosure. Using these data sets, we studied people’s self-disclosure on social media in terms of symptomatic mental health concerns and expressions of support. We employed transfer learning classifiers that identified the social media language indicative of mental health outcomes (anxiety, depression, stress, and suicidal ideation) and support (emotional and informational support). We then examined the changes in psychosocial expressions over time and language, comparing the 2020 and 2019 data sets.
Results: We found that all of the examined psychosocial expressions have significantly increased during the COVID-19 crisis—mental health symptomatic expressions have increased by about 14%, and support expressions have increased by about 5%, both thematically related to COVID-19. We also observed a steady decline and eventual plateauing in these expressions during the COVID-19 pandemic, which may have been due to habituation or due to supportive policy measures enacted during this period. Our language analyses highlighted that people express concerns that are specific to and contextually related to the COVID-19 crisis.
Conclusions: We studied the psychosocial effects of the COVID-19 crisis by using social media data from 2020, finding that people’s mental health symptomatic and support expressions significantly increased during the COVID-19 period as compared to similar data from 2019. However, this effect gradually lessened over time, suggesting that people adapted to the circumstances and their “new normal.” Our linguistic analyses revealed that people expressed mental health concerns regarding personal and professional challenges, health care and precautionary measures, and pandemic-related awareness. This study shows the potential to provide insights to mental health care and stakeholders and policy makers in planning and implementing measures to mitigate mental health risks amid the health crisis.
Introduction
The impacts of global public health emergencies extend beyond medical repercussions; they affect individuals and societies on many levels, causing disruptions [ 1 , 2 ]. In an article written by the American Psychological Association following the Ebola outbreak [ 3 ], the epidemic was described as an “epidemic of fear.” In the United States, it was labeled by the media as “fearbola” to describe a paranoia that infected the country. Reports of similar feelings of anxiety, stress, and uncertainty have been repeatedly reported during other global outbreaks and pandemics [ 4 ]. The ongoing outbreak of SARS-COV-2 has led to a pandemic of illness (COVID-19) that has caused 16 million cases and 700,000 deaths worldwide, reported as of the end of July 2020 [ 5 ]. According to recent surveys from the Census Bureau, the Centers for Disease Control and Prevention, and other studies, the COVID-19 crisis has been reported to be associated with rapid rises in psychological distress across many nations [ 6 ], with women, the young, the less educated, and some ethnic minority groups reporting greater mental health strain [ 7 ]. On the one hand, people are worried about the direct effects of potential infection, including fears of death, lasting disabilities, or exacerbating chronic illnesses. On the other hand, actions to mitigate the spread of COVID-19, including social distancing, quarantines, and business closures with resulting job losses, are a source of life disruptions and emotional distress.
Fear and anxiety about a disease as infectious as COVID-19 can trigger new-onset or exacerbate existing mental illness [ 8 ]. Therefore, the practical impact of the crisis is far greater than the actual number of infection cases or fatalities [ 8 , 9 ]. Although expressions of distress may stem from concern and worry relating to the direct impacts of the disease, they may relate as much to disruption of regular routines, sleep and eating patterns, having children out of school and at home full-time, economic hardships and unusual volatility in financial markets, and forced geographical displacement or confinement. Indeed, some people are at risk of developing posttraumatic distress due to exposure to the multifaceted uncertainties or from confronting dying people or lost loved ones. Although disease mitigating efforts such as “social distancing” and “self-quarantining” are recommended [ 10 - 12 ], individuals in medical isolation may experience increased symptoms of anxiety and depression, as well as feelings of fear, abandonment, loneliness, and stigmatization [ 13 , 14 ].
Despite concerns about the myriad of social and behavioral issues associated with the COVID-19 pandemic [ 15 , 16 ], there has been scant research to examine its psychosocial impacts or how to predict and mitigate them. Although it is anticipated that COVID-19 will have broadly ramifying effects [ 17 , 18 ], public health workers and crisis interventionists are limited in their ability to extend services and support in a timely, preemptive fashion. Although surveys are a step forward to support such efforts [ 7 ], due to their retrospective recall bias, limited scalability, and inability to provide real-time insights, public health workers are not only unable to prioritize services for the most vulnerable populations but also, more specifically, less equipped to direct prevention efforts toward individuals with greater propensities for adverse psychological impacts.
This paper seeks to address the aforementioned gap by drawing insights into people’s expressed mental health concerns by leveraging social media data. The rise in online and social media activity has provided an unprecedented opportunity to enhance the identification and monitoring strategies of various mental and psychosocial disorders [ 7 , 19 ]. Over 80% of US adults use social media daily [ 20 ], placing it ahead of texting, email, and instant messaging, and disclose considerably more about themselves online than offline [ 21 , 22 ]. Social media provides a real-time platform where people often candidly self-disclose their concerns, opinions, and struggles during this pandemic [ 23 ]. In particular, our study targets the following research aims:
- Aim 1: To quantitatively assess the psychosocial effects of the COVID-19 pandemic using social media data
- Aim 2: To examine how the psychosocial effects of the COVID-19 pandemic have varied over time
- Aim 3: To examine if social media language reflects the major psychosocial concerns during the COVID-19 pandemic
For these research questions, we measured psychosocial effects in terms of symptomatic mental health expressions of anxiety, depression, stress, and suicidal ideation, and expressions seeking emotional and informational support. Our study is founded on a large body of work on studying mental health and psychosocial dynamics with social media data [ 24 - 30 ]. Several studies have leveraged Twitter (which is also the data we used) to study health attributes and public health [ 30 ], including symptoms related to diseases [ 31 ], disease contagion [ 32 ], obesity and physical health [ 33 ], mood and depressive disorders [ 28 , 34 ], mental health self-disclosures [ 27 ], posttraumatic stress disorder [ 35 ], addictive behaviors and substance use [ 36 , 37 ], etc. Because social media data (and Twitter posts in particular) are recorded in the moment, they provide rich information about both the individual as well as the larger world [ 30 ]. In particular, we draw on two kinds of prior work: symptomatic mental health expressions and support expressions. Related to the former, Saha et al [ 25 ], in their study on the effects of psychiatric medications on Twitter, developed classifiers of mental health symptomatic expressions using social media language, which we replicated in this study. Related to the latter, we draw upon Sharma and De Choudhury’s [ 38 ], and Saha and Sharma’s [ 39 ] developed classifiers of social support expressions, specifically emotional and informational support.
Using Twitter Data
To study people’s psychosocial expressions on social media, we obtained Twitter data. Twitter is one of the most popular social media platforms, and its public-facing, microblogging–based design enables candid self-disclosure and self-expressions for individuals [ 27 ].
Twitter Streaming Application Programming Interface
We collected data in our study using the Twitter Streaming application programming interface (API). The Twitter Streaming API is an official data collection API that Twitter shares with researchers providing free access to a 1% sample of its data on parameters set by researchers. That is, for a given set of parameters, Twitter queries the volume of available data at a particular moment [ 40 ]. If the volume of the query exceeds 1% of all Twitter posts at that moment, then the response is sampled to be less than 1%. However, the Twitter Streaming API is like a black-box with a lack of transparency in the sampling methodology [ 41 , 42 ], yet this is one of the few forms of unfettered and large-scale social media data access to researchers outside social media companies [ 43 ] and has been used in prior research, including in health-related studies [ 35 , 44 , 45 ]. The Discussion section revisits the limitations of our study due to the challenges of the Twitter Streaming API.
For the purposes of our study, we used two kinds of parameters: (1) language of a Twitter post as “english” and (2) geolocation bounds set to be within the geographic coordinates of the United States. Therefore, our following analyses concern Twitter data that at least fulfill both these criteria. We note that the location filter additionally prevents any retweets in the data set, as retweets are not geolocation labeled by design on Twitter [ 40 ], allowing us to study only originally created Twitter posts.
Treatment Data
In particular, we focused our study on the US population and leveraged the Twitter Streaming API. Using geo-bounded coordinates, we collected 1% of real-time Twitter data originating from the United States. We collected 59,096,694 Twitter posts between March 24, 2020, and May 24, 2020. Because this data set comes from the same period when the COVID-19 outbreak occurred, we labeled this data set as the treatment data set. We note that this period saw an exponential growth in reported COVID-19 infection cases (about 50,000-1 million) and fatalities (about 1000-56,000) in the United States [ 46 ]. During these 2 months, federal and state policies and laws were enacted to control or mitigate the spread of the outbreak, including school and work closures; stay-at-home orders; and the Coronavirus Aid, Relief, and Economic Security Act [ 47 ].
Control Data
To understand the social media expressions particularly attributed to the COVID-19 crisis, we obtained a control data set that originated from the same geographical location (the United States) and a similar time period but from the previous year (2019). Prior work [ 47 , 48 ] motivated this approach of obtaining control data that acts as a baseline and likely minimizes confounding effects due to geo-temporal seasonality in lifestyle, activities, experiences, and unrelated events that may have some psychosocial bearing. We obtained a similarly sized data set of 40,875,185 Twitter posts shared between March 24, 2019, and May 24, 2019.
Both the treatment and control data sets were collected in real time, and therefore, they were the entire 1% sample of Twitter posts returned in real time; we did not conduct any additional sampling on this data. We note that the size of the control data was smaller than that of the treatment [ 42 ] despite each consisting of the same 2-month duration. This could be because the volume of posts [ 40 , 42 ] on Twitter increased significantly in 2020 [ 49 ], leading to an increase in the 1% sample as well. However, we cannot make any such conclusion, especially because of the lack of transparency in how Twitter conducts the 1% sampling [ 42 ].
Psychosocial Effects of COVID-19
Study design.
Toward our first research aim of understanding the psychosocial impacts of the COVID-19 outbreak, we conducted two types of analysis on our Twitter data set, which we describe in the following sections. Our study builds upon the vast, rapidly growing literature studying mental health concerns and psychosocial expressions within social media data [ 19 , 21 , 24 - 28 , 34 , 48 , 50 - 52 ]. We adopted a quasi-experimental study design, which minimizes for geo-temporal confounds by using Twitter data sets from similar regions and similar times of the year in a treatment (2020) and a control (2019) year.
Symptomatic Mental Health Expressions
Drawing on the work previously referenced, we hypothesize that people’s self-disclosure expressions on social media can reveal symptomatic mental health expressions attributed to the COVID-19 crisis. We examined symptomatic expressions of anxiety, depression, stress, and suicidal ideation. These are not only some of the most critical mental health concerns but also have been attributed to be consequences of the pandemic outbreak [ 15 , 53 , 54 ].
To identify mental health symptomatic expressions in social media language, Saha et al [ 25 ] built machine learning classifiers using transfer learning methodologies—the main idea here is to infer mental health attributes in an unlabeled data by transferring a classifier trained on a different labeled data set. These classifiers are n -gram–based ( n =1,2,3) binary support vector machine (SVM) models, where the positive class of the training data sets stems from appropriate Reddit communities ( r/depression for depression, r/anxiety for anxiety, r/stress for stress, and r/SuicideWatch for suicidal ideation), and the negative class of training data sets comes from nonmental health–related content on Reddit—a collated sample of 20 million posts gathered from 20 subreddits from the landing page of Reddit during the same period as the mental health subreddit posts, such as r/AskReddit , r/aww , and r/movies . These classifiers perform at a high accuracy of approximately 0.90 on average on held-out test data [ 25 ].
Clinical Validity
Saha et al’s [ 25 ] classifiers used here have also been shown to transfer well on Twitter with an 87% agreement between machine-predicted labels and expert appraisal [ 48 ], where experts annotated posts in the classification test data using Diagnostic and Statistical Manual of Mental Disorders, 5th Edition [ 55 ] criteria of mental health symptoms. Bagroy et al [ 56 ] reported additional validation of such derived insights with feedback from clinical experts [ 55 ]. In this study, the outcomes of the mental health expression classifiers were compared with those given by human coders on the same (random) sample of social media posts; the latter coded the posts based on a codebook developed using prior qualitative and quantitative studies of mental health disclosures on social media and literature in psychology on markers of mental health expressions. Coders not only agreed with the outcomes of the classifiers (κ=0.83) but also noted that the classifiers could identify explicit expressions of firsthand experience of psychological distress or mental health concerns (“i get overwhelmingly depressed”) as well as expressions of support, help, or advice around difficult life challenges and experiences (“are there any resources I can use to talk to someone about depression?”). Further details about these classifiers, including their detailed performance, predictive features demonstrating model interpretability, and efficacy of transfer to Twitter data, can be found in [ 25 , 48 , 56 ]. We used these classifiers to machine label both our treatment and control data sets. Textbox 1 shows example Twitter posts in our data set that exhibit mental health symptomatic expressions (because many of these labels were comorbid, we show example posts that exhibit one or more of these mental health symptomatic expressions).
Example paraphrased posts in the treatment data that exhibited high symptomatic mental health expressions.
- I am so sick and tired of the #coronavirus (anxiety, stress)
- The kind of person I am, I don’t deserve to meet these people (depression)
- 2020 is the saddest year. There is a lack of money, necessities needed for daily life are gone from stores! I am at work as a healthcare professional hurting for my patients because they can’t see their family. (anxiety, stress)
- I am too overwhelmed by school and having a crippling anxiety to keep up with everything online I’m seriously NOT OK! I CAN’T TAKE THIS! (anxiety, suicidal ideation)
- During the online lecture, the prof. asked each of us how we were doing and feeling, I said, I am too anxious to know what’s next, and i keep thinking about what’s gonna happen, and she was like okay chill! (depression, anxiety, stress)
Support Expressions
Social support is considered an essential component in helping people cope with psychological distress [ 57 ]. Research reports that supportive interactions can even have a “buffering effect” [ 57 , 58 ]; that is, they can be protective against the negative consequences of mental health. With the wide adoption of web and social media technologies, support seeking (and providing) is increasingly happening online and has been shown to be efficacious [ 21 , 59 ]. In fact, a meta-analysis indicated that online support is effective in decreasing depression and increasing self-efficacy and quality of life [ 60 ]. In the context of suicide, certain types of social support in Reddit communities may reduce the chances of future suicidal ideation among those seeking mental health help [ 61 ]. Oh et al [ 62 ] further showed that surveyed Facebook users demonstrated a positive relationship between having health concerns and seeking health-related social support. Indeed, during global crises such as COVID-19, when many of the physical sites for health care (including mental health) have been closed or have restricted access, it is likely that online support has proliferated [ 63 ]. Fear of potential infection may further have alienated individuals in need to pursue formal treatment, therapy, and support, perhaps channelizing their support-seeking efforts online and on social media.
According to the “Social Support Behavioral Code” [ 64 ], two forms of support that have received theoretical and empirical attention are emotional and informational support. Emotional support (ES) corresponds to empathy, encouragement, and kindness, while informational support (IS) corresponds to information, guidance, and suggestions [ 38 , 65 ]. These two forms of support have been found to be most prevalent and effective in several studies of online support and social media [ 38 , 62 , 66 , 67 ]. Social media enables individuals to self-disclose and express their emotional and informational needs [ 67 ]. Andalibi et al [ 66 ] found that these two kinds of support can co-occur with other forms of support, such as posts seeking ES often seeking esteem and network support, and Attai et al [ 68 ] noted that Twitter is effective in seeking and providing health-related informational needs, contextually related with our problem of interest.
To identify support expressions on social media, we used an expert-appraised data set and classifier built in prior studies [ 38 , 39 ]. These are binary SVM classifiers identifying the degree (high and low) of ES and IS in social media posts. When the predictions of these classifiers were cross-validated with expert annotations from Sharma and De Choudhury’s [ 38 ] data, the classifiers were found to have k -fold cross-validation accuracies of 0.71 and 0.77 in ES and IS classifications, respectively [ 39 ]. Similar to the symptomatic expressions classifiers, the classifiers of support expressions are transferred from Reddit and typically performed well in our data set due to the high linguistic equivalence between Reddit and Twitter data sets [ 34 ]. We further manually inspected a random set of 125 Twitter posts in our data set using the methods outlined in prior studies [ 25 , 56 ] to rate each Twitter post with binary high or low ES and IS. We found that the manual ratings and classifier ratings showed a high agreement of 88% and 93%, respectively, indicating statistically significant transfer classification on Twitter. We used these classifiers to label the presence of ES and IS in our treatment and control data sets. Textbox 2 shows a few example paraphrased posts of support expressions in our treatment data set.
Example paraphrased posts in the treatment data on support expressions.
- To our residents, the town is here for you but we need your help if we are going to keep our hospitals from being overwhelmed. (emotional and informational support)
- I hope you are safe and healthy! Keep the faith God never fails us & always has perfect plan. (emotional support)
- my wife is laid off. She has been trying for days to get ahold of unemployment. Please help. We need income. Running low on basic things. (emotional and informational support)
- Dear God, we are going through some struggles these days. Could you please send us some sunshine? Thanks so much. (emotional support)
- According to my mom, kindness is needed more than ever now. So, send love to you! How are you being kind to others today? (emotional support)
Examining Psychosocial Expressions Over Time and Language
Approach overview.
Next, we describe the methods to examine how the COVID-19 pandemic may have caused changes in psychological expressions by comparing our treatment (outbreak year) and control (no outbreak year) data sets. For both our data sets, we aggregated the number of posts that expressed symptomatic and support expressions by day and by type. We compared the pervasiveness of each kind of measure in the data sets along with conducting statistical significance in their differences using two-sample t tests and effect sizes (Cohen d ).
Temporal Variation
For our second research aim, we compared the daily variation of measures between the treatment and control data sets, we transformed our data into standardized z scores. Our data sets relied on the Twitter Streaming API and were subject to daily inconsistencies of available data each day [ 41 ]. Transformed z scores are not sensitive to such absolute values and inconsistencies, and essentially quantify the number of SDs by which the value of the raw score is above or below the mean. Similar standardization techniques have been adopted in prior social media time series studies [ 48 , 69 ]. Z scores were calculated as (x − μ) / σ , where x is the raw value, μ is the mean, and σ is the SD of the population. Here, to obtain population μ and σ , in addition to our treatment and control data, we also included a year-long Twitter data of over 240 million Twitter posts (September 2018 to August 2019). For each of the measures in symptomatic and support expressions, we first calculated μ and σ on the per-day occurrence of that particular measure in the data set of over 300 million Twitter posts (combining 240 million posts between September 2018 and August 2019, and 60 million posts in the treatment data between March and May 2020). For each measure, we then calculated the z score per day and interpreted the positive z scores as values above the mean and negative z scores as those below the mean.
Linguistic Differences
For our third research aim, we examined COVID-19–related linguistic differences in the psychosocial expressions on social media, we employed an unsupervised language modeling technique, the Sparse Additive Generative Model (SAGE) [ 70 ]. Given any two data sets, SAGE selects salient keywords by comparing the parameters of two logistically parameterized-multinomial models using a self-tuned regularization parameter to control the trade-off between frequent and rare keywords. We conducted SAGE to identify distinguishing n -grams ( n =1,2,3) between the treatment and control data sets, where each n -gram was returned with a SAGE score. The magnitude of an n -gram’s SAGE score signals the degree of its “uniqueness” or saliency, and in our case, a positive SAGE score (above 0) indicated that the n -gram was more salient in the treatment data, whereas a negative SAGE score (below 0) denoted greater saliency in the control data.
SAGE allowed us to obtain how the expressions differ during the COVID-19 outbreak as compared to the control period. We conducted two SAGE analyses, one each for symptomatic and support expressions. For the symptomatic expressions, we first obtained posts that were indicative of either anxiety, depression, stress, or suicidal ideation in the treatment and control data sets, and obtained SAGE for both. We used a similar method for support expressions by obtaining posts that were indicative of either emotional or informational support.
Finally, we cross-examined the salient keywords across symptomatic and support expressions to study how concerns were prevalent in either or both of the expression types. We measured log-likelihood ratios (LLRs) along with add-one smoothing, where LLRs close to 0 indicated comparable frequencies, LLRs<1 indicated the greater frequency in symptomatic expressions, and LLRs>1 indicated the greater frequency in support expressions. Together, these linguistic analyses enabled us to obtain psychological concerns and understand how COVID-19 has psychosocially affected individuals, and to contextualize these concerns in the literature on consequences of global crises.
Summary of Results
We summarize our first set of results in Table 1 . For all our measures, we found statistical significance (as per t tests) as well as significant effect sizes (Cohen d >0.4 for all measures [ 71 ]) in social media expressions in the treatment data as compared to that in the control data. Assuming that most other confounders were minimized due to the geo-temporal similarity of the data sets, our findings indicated that the COVID-19 outbreak led to an increase in people’s symptomatic and support expressions of mental health. We elaborate on the results in the following sections.
Figure 1 shows the changes in symptomatic mental health expressions for the same period in the treatment (2020) and control (2019) years. We found that the treatment and control data sets showed significant differences in people’s symptomatic expressions ( Table 1 ), among which anxiety showed the most significant increase (21.32%), followed by suicidal ideation (19.73%), depression (10.18%), and stress (3.76%). Figure 2 shows the evolution of support expressions change in the treatment and control data sets. The differences were significant ( Table 1 ), and we found that ES increased by 4.77% and IS increased by 4.78%.

In both the plots of Figures 1 and 2 , we found a general trend of negative slope (average slope=–0.03) within the treatment year, which was closer to zero slope (average slope=3.19*10 −4 ) in the control data set. This may suggest that within the treatment year, people’s mental health expressions gradually leveled out over time, despite the growing rate of COVID-19 active cases. The plots indicated that psychological expressions almost converge at the tails. This could likely be due to people’s habituation with the situation and surroundings with the passage of time [ 70 , 72 ], as has been observed for other crisis events [ 48 , 73 ]; however, this needs to be explored further. Within the control data set, we observed a sudden peak on April 28, 2019, which could be attributed to a shooting incident at a synagogue in San Diego [ 74 ]. The observations reflected that the COVID-19 pandemic has increased people’s mental health expressions on social media, aligning with other contemporary literature and media reports [ 8 , 53 ].
Linguistic Expressions
Table 2 summarizes the language differences as per SAGE for posts expressing high mental health expressions in the treatment and control periods—keywords with positive SAGE saliently occurred in the treatment data, whereas those with negative SAGE saliently occurred in the control data. A majority of the keywords that occurred in the treatment period were contextually related to the COVID-19 pandemic, such as covid19 , coronavirus , social distancing , and stayathome isolation . These keywords were used in posts expressing mental health concerns either explicitly (eg, “Social distancing is both sad and anxiety-inducing at the same moment”) or implicitly (eg, “In order to get my family treated, I will do more than beg, and I will donate 25K for research to develop COVID19 vaccine”). We also found that the treatment period used keywords referring to key personnel such as dr fauci (referring to Anthony Fauci, one of the leads in the incumbent White House Coronavirus Task Force in the United States and Director of the National Institute of Allergy and Infectious Diseases since 1984 [ 75 ]) and political figures like Nury Martinez and Donald Trump . Further, we found keywords such as essential workers , doctor jobs , and risking lives , which describe high-risk worker situations (eg, “I am not complaining about going to work, rather, I am concerned about risking my health for work”), and certain treatment suggestions that evolved during this period [ 76 ], such as garlic , malaria , and hydroxychloroquine (eg, “I do worry tho! He is focused on job numbers, approval? ratings and repeating mistruths. His spouting of 2 drugs, one for malaria & the other a Z-pack. A Senior couple tried these untested drugs; wife is in ICU & husband also hospitalized! This is irresponsible & dangerous!”).
a SAGE: Sparse Additive Generative Model.
b Positive SAGE scores indicated greater saliency in the treatment (2020) data.
c Negative SAGE scores indicated greater saliency in the control (2019) data.
Table 3 lists the top keywords as per SAGE for support posts in the treatment and control periods. Keywords with positive SAGE saliently occurred in the treatment data, whereas those with negative SAGE saliently occurred in the control data. We found keywords that explicitly relate to COVID-19 occurred in the treatment period. We also found that the treatment period consisted of posts that seek support related to job and pay, such as losing jobs , need pay , and furloughed (eg, “Many in our community have lost their jobs, are underinsured and are struggling to make ends meet. Providing pantries, hot meals, hotspots and distance learning opportunities is now more critical than ever, please donate”). Our data also revealed the prevalence of contextually related keywords such as masks , ppe , hoarding , stockpile , and sanitizer that are medically recommended prevention and containment measures of COVID-19 infection (eg, “Please contact me if you have any N95 mask or know to obtain some. My sister and a few friends work in the OR and they do not have the supplies to stay safe, they have patients who have #COVID19. TY! #HealthcareHeroes”).
Linguistic Comparability
Finally, Table 4 shows the results of the lexical comparability analysis, where LLRs demarcate the top keywords used for symptomatic mental health expressions and support expressions within the treatment data set. We found that keywords, such as safety precautions ( wear masks ), health care and treatment ( health care workers, hospitalized, beds, and icu ), and life and death ( passed away, kill people, human lives, and deaths ), comparably overlapped in both kinds of psychological expressions (LLRs~0). These keywords were also used to raise awareness and express solidarity with health care and high-risk workers (eg, “Taking all safety precautions and adhering to the guidelines established by our health care professionals will keep us safe”). Our lexico-psychological analyses revealed that more clinically relevant keywords and symptoms occurred frequently in symptomatic expressions (LLRs>0; eg, sleep schedule and tested positive ), whereas socially relevant and stressful circumstances were more prevalent in support expressions (LLRs<0; eg, im single parent, starve, and lost jobs ).
a LLR: log likelihood ratio.
b Keywords with LLRs>0 distinctly occurred in high symptomatic expressions.
c Keywords with LLRs~0 occurred comparably in both symptomatic and support expressions.
d Keywords with LLRs<0 distinctly occurred in support expressions.
Principal Results
Our study suggests that social media posts during the COVID-19 pandemic contain a significantly higher frequency of symptomatic mental health and support expressions than a comparable data set from the same period in the previous year. The effect sizes and statistical differences observed in our analyses provide evidence that COVID-19 may have led to mental health concerns compared to other normative times. We also found that they topically relate to the ongoing crisis situation and include concerns such as treatment, precautionary measures, loss of jobs, school closings, stockpiling of basic livelihood necessities, feeling lonely, boredom, and tired of the restrictions and constraints put on by the ongoing pandemic. Our findings suggest that although the COVID-19 pandemic has amplified mental health risks and concerns, it may have heightened a sense of belonging and solidarity among individuals—bringing them together, raising collective awareness, and encouraging them to provide support to one another. We also found expressions of solidarity with health care and high-risk workers, suggesting that people have been considerate about these workers and have expressed desire to set up opportunities for donating to those who have lost jobs during the crisis; this also aligns with recent media reports and World Health Organization guidelines of tackling the pandemic [ 77 , 78 ]. Media reports have also indicated how benevolent neighbors have been, tending to their older adult neighbors by delivering their groceries and other basic necessities [ 79 ].
However, mental health experts say that, although the crisis is amplifying risk factors for suicide, the COVID-19 outbreak’s effect on individuals’ mental and emotional well-being is complex [ 80 ]. Suicide is multifaceted, and although economic loss is a risk factor, so are depression, isolation, and fear of the future. At the same time, the crisis is possibly creating a sense of belonging for individuals at risk for suicide, as stress and anxiety are normalized, and people come together to better support one another during a crisis [ 81 , 82 ]. Our data showed a significant impact of COVID-19 on suicidal ideation, which calls for enhanced importance of population-scale mental health care, such as using approaches like universal screening (ie, Zero Suicide Model) [ 83 ]. As Florida [ 84 ] noted in a recent article, “The long-term toll on mental health of social isolation, remote work, and economic insecurity could have impacts akin to post-traumatic stress disorder; yet, the new focus on mental health may reduce stigma and increase the availability of support services.” Indeed, the world beyond the crisis may be one in which mental health is more honestly recognized and supported.
Interestingly, we noted that our findings indicate a gradual leveling out of these expressions, both symptomatic and supportive, which may reflect a developing new normal . In February 2020, it seemed unthinkable that the white-collar workforce of many countries would soon be working solely from home; it seemed unthinkable that air travel would plummet by 96% and that all major sporting events would be called off. Indeed, epidemiologists surmise that many if not most of the changes surrounding the rhythms of our daily life are likely to fade over time, just as they did after the 1918 influenza epidemic [ 84 ]. In other words, the pandemic could make us revisit and possibly reform many of our lifestyle choices and civic roles, and the persistent discussion of the new normal may help bring order to our current turbulence. Others have argued that perhaps the crisis is a prelude to a new paradigm , as recently noted by the World Economic Forum [ 84 , 85 ]: “Feeling unsettled, destabilized and alone can help us empathize with individuals who have faced systematic exclusions long-ignored by society even before the rise of COVID-19 – thus stimulating urgent action to improve their condition.” We should, therefore, “revel in the discomfort of the current moment to generate a ‘new paradigm,’ not a ‘new normal.’” The leveling out trend in our data gives empirical ground to these conjectures.
Nevertheless, if robust antiviral treatments are developed and rolled out relatively quickly or if a vaccine becomes available soon enough, presumably, the changes will be short-lived, and the new normal may be temporary. However, if the pandemic comes back in larger waves over the next few seasons, as was the case with historical epidemics, the economic, political, and social crises that have arisen as a consequence will lead to deeper ramifications in turn, leading to longer lasting or permanent changes. Future research will need to explore the persistence of the new normal and the emergence of a possible new paradigm as the pandemic evolves, and therein the mental health impacts further along in the crisis. A study like ours on the ongoing pandemic is a step toward leveraging large-scale online data to understand people’s response to the crisis and thinking about means to address the major concerns. Our study bears implications in digital technology driven mental health interventions to provide tailored support to people’s concerns during the crisis; a recent work by Rudd and Beidas [ 86 ] pointed out four point guidelines to build innovative and expansive solutions toward improving public mental health. The variety of concerns and help-seeking factors reflected in our study can also help several stakeholders, ranging across mental health facilitators and policy makers, toward early preparedness and interventions for mental health support. Similarly, our methods can offer the potential to build public health surveillance technologies that surface early warning signs of the effects of the various events related to the pandemic and other crises. The potential of social media to assist in the response to the pandemic is clear but also dependent on the accuracy of underlying methods. The reach of social media allows for broad access that transcends national borders or cultural differences. Using this access to meet the increasing need for help seeking, online and social media data is in a prime position to offer people personalized guidance toward accurate information, health care resources, and even basic lifestyle interventions. Underlying this potential is, thus, the ability of social media data to classify the state and needs of each individual and use that information to tailor a customized response. Precedents for such a system are abound as seen in several prior studies [ 27 - 31 , 37 , 87 - 89 ].
Comparison With Prior Work
COVID-19 is not the first pandemic—catastrophic pandemics have been occurring at regular intervals throughout human history, with the 1918 influenza epidemic being the last one before the current pandemic [ 84 , 85 , 90 ]. The backdrop of the 1918 pandemic was that it happened just before the advent of modern psychiatry as a science and a clinical specialty—a time when psychoanalysis was gaining recognition as an established treatment within the medical community [ 91 , 92 ]. Consequently, psychiatry has had little opportunity to consider such historically important phenomena through its clinical, scientific lens until now. Although outbreaks of the Zika and Ebola viruses, Middle East respiratory syndrome, and severe acute respiratory syndrome managed to draw global attention, stirring up anxiety and uncertainty in societies, scholars have noted that participation of mental health experts in pandemic preparedness has remained negligible [ 93 ]. Consequently, our ability to understand mental health responses as well as the mental health burden in pandemic outbreaks have been limited [ 94 ]. For instance, a routinely practiced method of infection control, quarantine and social distancing, have received surprisingly little attention in psychiatric literature so far. Baumeister and Leary [ 95 ] contended that humans need frequent contacts, and crisis events further stimulate a need for affiliation and intimacy. Therefore, prolonged isolation and separation from families and their community can have profound effects on individuals even if they are not directly affected by the disease [ 4 ]. In the current pandemic, the additional layer of extensive social media use and exposure to often sensationalized online news while in physical isolation may add new complexities to implementing emotional epidemiology in managing concerns, fears, and misconceptions [ 96 , 97 ], as these tools have been argued to bear negative effects on psychological well-being [ 97 , 98 ].
By adopting social media as a lens to unpack these previously less understood dimensions of a pandemic’s mental health effects, our study is one step toward closing some of the previously noted gaps. The published literature posits that the distress and anxiety among individuals in this COVID-19 pandemic may increase the incidence of mental disorders [ 53 , 54 , 99 ]; data thus far from the United States point to a population increase in psychological distress of 10% compared to 2018 data [ 8 ], a trend that is in line with our results. These rates may be higher in those regions heavily exposed to COVID-19 or among individuals working during the pandemic, with a recent review reporting over 20% prevalence of anxiety, which is also consistent with our findings [ 8 ].
Prior work found that mental health discourse on Twitter ranges across stigmatizing, inspirational, resource, medical, and social dimensions of expressions [ 100 ], and our study revealed similar topical diversity in our data set. Further, we detected through social media many of the stresses associated with the pandemic (eg, prolonged isolation, exposure to pandemic-related death, loss of income and career, increased workload, and lack of pertinent and accurate information). These results align with epidemiological findings that COVID-19 has led to elevated mental health symptoms for individuals. Nelson et al [ 101 ] surveyed 2000 individuals from the United States, Canada, and Europe, and found elevated symptoms of anxiety and depression compared to historical norms and observed factors similar to the concerns we detected regarding symptomatic expressions and those related to seeking support. They also reinforced the summary data released by the Crisis Text Line (a major crisis helpline in the United States) listing major concerns of crisis support sought during this period [ 102 ], with 80% of conversations mentioning “virus,” 34% mentioning “anxiety,” 34% feeling solidarity with friends and family, etc. Along similar lines, there have been numerous reports about the increasing number of mental health crisis helpline calls during this period [ 103 , 104 ], providing further support and external validation that our social media findings reflect many of the same elements of distress expressed offline during this crisis.
Next, our temporal analyses pointed to a steady decline in people’s expressed psychosocial concerns during the 2-month study period ( Figures 1 and 2 ), which conforms with similar findings in Google search queries as stay-at-home orders and other COVID-19–related policy changes were implemented in the United States [ 105 ]. We note contemporary social computing research studying various aspects of the social media discourse related to COVID-19 [ 63 , 106 - 108 ]. By providing complementary evidence to observations by Mackey et al [ 106 ] and Stokes et al [ 107 ] on expressed (mental health) concerns during the crisis, our study further underscores their findings using a comparable (control) data set, reinforcing and providing empirical credibility to the impression that the COVID-19 pandemic has indeed caused or contributed directly to the mental health concerns that we describe.
Limitations and Future Work
We note some limitations in our study, many of which present excellent directions for future research. We recognize the lack of transparency related to the Twitter Streaming API. Recent research has also questioned the credibility of the “1% Twitter stream” aspect, noting that actual sampling data was smaller than what it ideally should have been [ 41 ]. Given these data limitations, we decided against conducting several descriptive and fine-grained analyses (such as comparing regions), and refrained from making claims based on comparing absolute numbers of those impacted by various mental health concerns. For example, we cannot define based on our data whether there were increased or decreased Twitter postings during our COVID-19 study period compared to the same months in 2019. Again, we chose to filter English-only Twitter posts given both algorithmic limitations of our methodologies and lower prevalence of non-English data (particularly in the US context). However, future work can extend our methodologies to conduct analyses in other languages to draw richer insights.
Despite the strengths of Twitter as a data source that provides us unobtrusive access to large-scale, unstructured, and naturalistic data of people’s candid self-disclosure and that it has been a valuable source to study disaster and crisis response [ 109 ], we acknowledge that this data inherently has many biases such as self-selection and representation [ 110 ]. We can only study those who self-select to express on Twitter. Pew Internet Center surveys reported that social media platforms are underrepresentative of minorities, although Twitter is an exception, which overrepresents minorities such as Blacks, Hispanics, and women [ 20 ]. There is already a digital divide in terms of social media use where the population is skewed toward young adults and white-collar workers. Further, technology and social media could be a luxury to marginalized and underprivileged populations, and any sort of technology-driven support and assistance will disproportionately affect different individuals based on technology use [ 88 ]. Similarly, a single platform cannot provide a complete picture; different platforms (eg, Facebook, Reddit, Twitter, and instant messaging services) have unique design strengths and weaknesses both in terms of their affordances as well as who uses them. Therefore, as highlighted in a recent article by Chunara and Cook [ 23 ], public health surveillance (including that for COVID-19) can account for several factors such as the “population at risk” in epidemiology and demographic disparities in the use and behavioral expressions on social media.
We understand that our study is observational and, as any other observational study, does not measure “true causality.” Watts [ 111 ] noted the impossibility to test all explanations and confounders simultaneously. However, by including and comparing against control data, we minimized geo-temporal and seasonal confounds, thereby enabling us to provide stronger evidence and insights than purely correlational analyses regarding the effects of the COVID-19 pandemic on people’s mental health. We also note that support expressions in our study can not only include support-seeking but also support-providing expressions. This has also enabled us to observe how solidarity and sense of belonging proliferated during the COVID-19 crisis. Future work can build separate high precision classifiers for each kind of expression to disentangle the prevalence of seeking and providing expressions during the crisis.
Further, although we did have data beyond May 24, 2020, we decided to exclude those to keep our focus on the effects on social media expressions due to COVID-19 and minimize those that followed the death of George Floyd on May 25, 2020, in the light of the Black Lives Matter protests throughout the United States [ 112 ]. We also are aware that, with the continuing nature of the pandemic, our conclusions are restricted to the mental health and support-seeking concerns expressed during a finite study period. Events since the end of the study period underscore the dynamic nature of these events, as different parts of the United States are heavily affected, while others are recovering, and some remain relatively spared. It will be important to extend this work temporally; increase the size of future samples; and, whenever possible, add geospatial specificity to future analyses. The latter will be especially important for potential supportive interventions locally if one has the resources and the ability to assemble recurring, near-real-time local “snapshots” as a basis for community-focused preventive interventions. Further, our analyses can be extended to retrospectively examine the aftereffects of particular global and local events, such as policy changes, related to the pandemic.
Our study, like those of others studying other major events, further reinforces the potential utility of accessing and analyzing social media data in near-real-time to take the temperature of communities. This will require a more focused and robust collection of locally targeted information to build samples that are sufficiently large to produce reliably representative data sets to be useful for public health interventions. Further work is now needed to track mental health–related expressions and those reflecting needs for support throughout the pandemic, which has seen dynamic changes associated with disease spread to areas that had been less affected during the early months of the outbreak. This geo-specific research may further enhance our understanding of the causal connections between COVID-19 spread and waves of expressed distress. Having the ability to present locally pertinent, contemporaneous analyses offers the opportunity for local public health and mental health providers as well as political leaders to develop and deploy targeted support services in a timely fashion.
Acknowledgments
MDC was partly supported by a COVID-19–related Rapid Response Research grant #2027689 from the National Science Foundation.
Conflicts of Interest
JT receives unrelated research support from Otsuka.
- Hays JN. Epidemics and Pandemics: Their Impacts on Human History. Santa Barbara, CA: ABC-CLIO; 2005.
- Boscarino JA. Community disasters, psychological trauma, and crisis intervention. Int J Emerg Ment Health 2015;17(1):369-371 [ FREE Full text ] [ Medline ]
- Lu S. An epidemic of fear. American Psychological Assocation. 2015. URL: https://www.apa.org/monitor/2015/03/fear [accessed 2020-07-25]
- Morganstein JC, Fullerton CS, Ursano RJ, Donato D, Holloway HC. 18 - pandemics: health care emergencies. In: Ursano RJ, Fullerton CS, Weisaeth L, Raphael B, editors. Textbook of Disaster Psychiatry. Cambridge, England: Cambridge University Press; 2017:270-284.
- COVID-19 coronavirus pandemic. Worldometers. URL: https://www.worldometers.info/coronavirus/ [accessed 2020-07-25]
- Basu T. The coronavirus pandemic is a game changer for mental health care. MIT Technology Review. 2020. URL: https://www.technologyreview.com/2020/03/20/905184/coronavirus-online-therapy-mental-health-app-teletherapy/ [accessed 2020-07-25]
- Resnick B. A third of Americans report anxiety or depression symptoms during the pandemic. Vox. 2020. URL: https://www.vox.com/science-and-health/2020/5/29/21274495/pandemic-cdc-mental-health [accessed 2020-07-25]
- McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA 2020 Jul 07;324(1):93-94 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Holmes EA, O'Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 2020 Jun;7(6):547-560 [ FREE Full text ] [ CrossRef ] [ Medline ]
- World Health Organization. Operational considerations for case management of COVID-19 in health facility and community. Interim guidance. Pediatr Med Rodz 2020 Jul 14;16(1):27-32. [ CrossRef ]
- Hellewell J, Abbott S, Gimma A, Bosse NI, Jarvis CI, Russell TW, Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group, et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health 2020 Apr;8(4):e488-e496 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Saxena SK, editor. Coronavirus Disease 2019 (COVID-19) Epidemiology, Pathogenesis, Diagnosis, and Therapeutics. Singapore: Springer; 2020.
- Miller G. Social distancing prevents infections, but it can have unintended consequences. Science 2020 Mar 17:1. [ CrossRef ]
- Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, Tenorio EL, CoroNerve Study Group. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatry 2020 Oct;7(10):875-882 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med 2020 Aug 06;383(6):510-512. [ CrossRef ] [ Medline ]
- Fiorillo A, Gorwood P. The consequences of the COVID-19 pandemic on mental health and implications for clinical practice. Eur Psychiatry 2020 Apr 01;63(1):e32 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Heymann DL, Shindo N, WHO Scientific and Technical Advisory Group for Infectious Hazards. COVID-19: what is next for public health? Lancet 2020 Feb 22;395(10224):542-545 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Weinstock CP. Ripple effects of COVID-19 strain mental health systems. US News. 2020. URL: https://www.usnews.com/news/healthiest-communities/articles/2020-06-04/coronavirus-ripple-effects-strain-mental-health-systems [accessed 2020-07-25]
- Chancellor S, De Choudhury M. Methods in predictive techniques for mental health status on social media: a critical review. NPJ Digit Med 2020;3:43. [ CrossRef ] [ Medline ]
- Social media fact sheet. Pew Internet Center. 2019. URL: https://www.pewresearch.org/internet/fact-sheet/social-media/ [accessed 2020-07-25]
- Andalibi N, Haimson OL, De Choudhury M, Forte A. Understanding social media disclosures of sexual abuse through the lenses of support seeking and anonymity. In: Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems. 2016 Presented at: CHI '16; May 2016; San Jose, CA. [ CrossRef ]
- Qiu L, Lin H, Leung AK, Tov W. Putting their best foot forward: emotional disclosure on Facebook. Cyberpsychol Behav Soc Netw 2012 Oct;15(10):569-572. [ CrossRef ] [ Medline ]
- Chunara R, Cook SH. Using digital data to protect and promote the most vulnerable in the fight against COVID-19. Front Public Health 2020;8:296. [ CrossRef ] [ Medline ]
- Guntuku SC, Schwartz HA, Kashyap A, Gaulton JS, Stokes DC, Asch DA, et al. Variability in language used on social media prior to hospital visits. Sci Rep 2020 Mar 12;10(1):4346. [ CrossRef ] [ Medline ]
- Saha K, Sugar B, Torous J, Abrahao B, Kıcıman E, De Choudhury M. A social media study on the effects of psychiatric medication use. Proc Int AAAI Conf Weblogs Soc Media 2019 Jun 07;13:440-451 [ FREE Full text ] [ Medline ]
- Saha K, Kim SC, Reddy MD, Carter AJ, Sharma E, Haimson OL, et al. The language of LGBTQ+ minority stress experiences on social media. Proc ACM Hum Comput Interact 2019 Nov;3(CSCW):1-22. [ CrossRef ] [ Medline ]
- Ernala SK, Labetoulle T, Bane F, Birnbaum ML, Rizvi AF, Kane JM, et al. Characterizing audience engagement and assessing its impact on social media disclosures of mental illnesses. 2018 Presented at: Twelfth International AAAI Conference on Web and Social Media; June 2018; Palo Alto, CA.
- De Choudhury M, Gamon M, Counts S, Horvitz E. Predicting depression via social media. 2013 Presented at: The 7th International AAAI Conference on Weblogs and Social Media; July 2013; Cambridge, MA.
- Saha K, Weber I, Birnbaum ML, De Choudhury M. Characterizing awareness of schizophrenia among Facebook users by leveraging Facebook advertisement estimates. J Med Internet Res 2017 May 08;19(5):e156 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Dredze M. How social media will change public health. IEEE Intell Syst 2012 Jul;27(4):81-84 [ FREE Full text ] [ CrossRef ]
- Paul MJ, Dredze M. You are what you tweet: analyzing Twitter for public health. 2011 Presented at: Fifth International AAAI Conference on Weblogs and Social Media; July 2011; Barcelona, Spain.
- Sadilek A, Kautz H, Silenzio V. Predicting disease transmission from geo-tagged micro-blog data. 2012 Presented at: Twenty-Sixth AAAI Conference on Artificial Intelligence; July 2012; Toronto, ON.
- Gore RJ, Diallo S, Padilla J. You are what you tweet: connecting the geographic variation in America's obesity rate to Twitter content. PLoS One 2015;10(9):e0133505 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Saha K, Chan L, De Barbaro K, Abowd GD, De Choudhury M. Inferring mood instability on social media by leveraging ecological momentary assessments. Proc ACM Interact Mob Wearable Ubiquitous Technol 2017 Sep 11;1(3):1-27. [ CrossRef ]
- Coppersmith GA, Harman CT, Dredze MH. Measuring post traumatic stress disorder in Twitter. 2014 Presented at: Eighth International AAAI Conference on Weblogs and Social Media; 2014; Ann Arbor, MI.
- Kiciman E, Counts S, Gasser M. Using longitudinal social media analysis to understand the effects of early college alcohol use. 2018 Presented at: 12th International AAAI Conference on Web and Social Media; June 2018; Palo Alto, CA.
- Liu J, Weitzman E, Chunara R. Assessing behavioral stages from social media data. CSCW Conf Comput Support Coop Work 2017;2017:1320-1333 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Sharma E, De Choudhury M. Mental health support and its relationship to linguistic accommodation in online communities. In: Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems. 2018 Presented at: CHI '18; April 2018; Montreal, QC. [ CrossRef ]
- Saha K, Sharma A. Causal factors of effective psychosocial outcomes in online mental health communities. Proc Int AAAI Conference Web Soc Media 2020;14(1):590-601.
- Filter realtime tweets. Twitter Developer. URL: https://developer.twitter.com/en/docs/twitter-api/v1/tweets/filter-realtime/guides/basic-stream-parameters [accessed 2020-08-17]
- Pfeffer J, Mayer K, Morstatter F. Tampering with Twitter’s sample API. EPJ Data Sci 2018 Dec 19;7(1):1. [ CrossRef ]
- Morstatter F, Pfeffer J, Liu H. When is it biased?: assessing the representativeness of twitter's streaming API. In: Proceedings of the 23rd International Conference on World Wide Web. 2014 Presented at: WWW '14 Companion; April 2014; Seoul, Korea. [ CrossRef ]
- Boyd D, Crawford K. Critical questions for big data. Inf Commun Soc 2012 Jun;15(5):662-679. [ CrossRef ]
- Burton SH, Tanner KW, Giraud-Carrier CG, West JH, Barnes MD. "Right time, right place" health communication on Twitter: value and accuracy of location information. J Med Internet Res 2012 Nov 15;14(6):e156 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Tsuya A, Sugawara Y, Tanaka A, Narimatsu H. Do cancer patients tweet? Examining the twitter use of cancer patients in Japan. J Med Internet Res 2014 May 27;16(5):e137 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Centers for Disease Control and Prevention. URL: https://www.cdc.gov/ [accessed 2020-05-09]
- Timeline of the COVID-19 pandemic in the United States. Wikipedia. URL: https://en.wikipedia.org/wiki/Timeline_of_the_COVID-19_pandemic_in_the_United_States [accessed 2020-07-25]
- Saha K, De Choudhury M. Modeling stress with social media around incidents of gun violence on college campuses. Proc ACM Hum-Comput Interact 2017 Dec 06;1(CSCW):1-27. [ CrossRef ]
- Iqbal M. Twitter revenue and usage statistics (2020). Business of Apps. 2020. URL: https://www.businessofapps.com/data/twitter-statistics/#2 [accessed 2020-08-17]
- De Choudhury M, Kiciman E, Dredze M, Coppersmith G, Kumar M. Discovering shifts to suicidal ideation from mental health content in social media. Proc SIGCHI Conf Hum Factor Comput Syst 2016 May;2016:2098-2110 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Guntuku SC, Ramsay JR, Merchant RM, Ungar LH. Language of ADHD in adults on social media. J Atten Disord 2019 Oct;23(12):1475-1485. [ CrossRef ] [ Medline ]
- Saha K, Weber I, De Choudhury M. A social media based examination of the effects of counseling recommendations after student deaths on college campuses. Proc Int AAAI Conf Weblogs Soc Media 2018 Jun;2018:320-329 [ FREE Full text ] [ Medline ]
- Bedford J, Enria D, Giesecke J, Heymann DL, Ihekweazu C, Kobinger G, WHO Strategic and Technical Advisory Group for Infectious Hazards. COVID-19: towards controlling of a pandemic. Lancet 2020 Mar 28;395(10229):1015-1018 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Taha S, Matheson K, Cronin T, Anisman H. Intolerance of uncertainty, appraisals, coping, and anxiety: the case of the 2009 H1N1 pandemic. Br J Health Psychol 2014 Sep;19(3):592-605. [ CrossRef ] [ Medline ]
- Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Washington, DC: American Psychiatric Association; 2013.
- Bagroy S, Kumaraguru P, De Choudhury M. A social media based index of mental well-being in college campuses. Proc SIGCHI Conf Hum Factor Comput Syst 2017 May;2017:1634-1646 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Kummervold PE, Gammon D, Bergvik S, Johnsen JK, Hasvold T, Rosenvinge JH. Social support in a wired world: use of online mental health forums in Norway. Nord J Psychiatry 2002;56(1):59-65. [ CrossRef ] [ Medline ]
- Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull 1985 Sep;98(2):310-357. [ Medline ]
- De Choudhury M, De S. Mental health discourse on Reddit: self-disclosure, social support, and anonymity. 2014 Presented at: Eighth International AAAI Conference on Weblogs and Social Media; May 2014; Ann Arbor, MI.
- Rains SA, Young V. A meta-analysis of research on formal computer-mediated support groups: examining group characteristics and health outcomes. Hum Commun Res 2009;35(3):309-336. [ CrossRef ]
- De Choudhury M, Kıcıman E. The language of social support in social media and its effect on suicidal ideation risk. Proc Int AAAI Conf Weblogs Soc Media 2017 May;2017:32-41 [ FREE Full text ] [ Medline ]
- Oh HJ, Lauckner C, Boehmer J, Fewins-Bliss R, Li K. Facebooking for health: an examination into the solicitation and effects of health-related social support on social networking sites. Comput Hum Behav 2013 Sep;29(5):2072-2080. [ CrossRef ]
- Luo C, Li Y, Chen A, Tang Y. What triggers online help-seeking retransmission during the COVID-19 period? Empirical evidence from Chinese social media. PLoS One 2020;15(11):e0241465 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Cutrona CE, Suhr JA. Controllability of stressful events and satisfaction with spouse support behaviors. Commun Res 1992;19(2):154-174. [ CrossRef ]
- Nambisan P. Information seeking and social support in online health communities: impact on patients' perceived empathy. J Am Med Inform Assoc 2011 May 01;18(3):298-304. [ CrossRef ] [ Medline ]
- Andalibi N, Haimson OL, Choudhury MD, Forte A. Social support, reciprocity, and anonymity in responses to sexual abuse disclosures on social media. ACM Trans Comput-Hum Interact 2018 Oct 17;25(5):1-35. [ CrossRef ]
- Wang YC, Kraut R, Levine JM. To stay or leave?: the relationship of emotional and informational support to commitment in online health support groups. In: Proceedings of the ACM 2012 conference on Computer Supported Cooperative Work. 2012 Presented at: CSCW '12; February 2012; Seattle, WA. [ CrossRef ]
- Attai DJ, Cowher MS, Al-Hamadani M, Schoger JM, Staley AC, Landercasper J. Twitter social media is an effective tool for breast cancer patient education and support: patient-reported outcomes by survey. J Med Internet Res 2015 Jul 30;17(7):e188 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Golder SA, Macy MW. Diurnal and seasonal mood vary with work, sleep, and daylength across diverse cultures. Science 2011 Sep 30;333(6051):1878-1881 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Eisenstein J, Ahmed A, Xing EP. Sparse additive generative models of text. 2011 Presented at: 28th International Conference on International Conference on Machine Learning; June 2011; Bellevue, WA.
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Taylor & Francis Group; 2013.
- Rankin CH, Abrams T, Barry RJ, Bhatnagar S, Clayton DF, Colombo J, et al. Habituation revisited: an updated and revised description of the behavioral characteristics of habituation. Neurobiol Learn Mem 2009 Sep;92(2):135-138 [ FREE Full text ] [ CrossRef ] [ Medline ]
- De Choudhury M, Monroy-Hernández A, Mark G. "Narco" emotions: affect and desensitization in social media during the mexican drug war. In: Proceedings of the SIGCHI Conference on Human Factors in Computing Systems. 2014 Presented at: CHI '14; April 2014; Toronto, ON. [ CrossRef ]
- Medina J, Mele C, Murphy H. One dead in synagogue shooting near San Diego; officials call it hate crime. The New York Times. 2019 Apr. URL: https://www.nytimes.com/2019/04/27/us/poway-synagogue-shooting.html [accessed 2020-07-25]
- Anthony S. Fauci, M.D. National Institute of Allergy and Infectious Diseases. URL: https://www.niaid.nih.gov/about/anthony-s-fauci-md-bio [accessed 2020-07-25]
- Colson P, Rolain J, Lagier J, Brouqui P, Raoult D. Chloroquine and hydroxychloroquine as available weapons to fight COVID-19. Int J Antimicrob Agents 2020 Apr;55(4):105932 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Mental health and psychosocial considerations during the COVID-19 outbreak. World Health Organization. 2020. URL: https://apps.who.int/iris/bitstream/handle/10665/331490/WHO-2019-nCoV-MentalHealth-2020.1-eng.pdf [accessed 2020-07-20]
- Broom D. A pandemic of solidarity? This is how people are supporting one another as coronavirus spreads. World Economic Forum. 2020. URL: https://www.weforum.org/agenda/2020/03/covid-19-coronavirus-solidarity-help-pandemic/ [accessed 2020-08-18]
- Free C. People across the country are delivering groceries free. It’s ‘solidarity, not charity.’. The Washington Post. 2020. URL: https://www.washingtonpost.com/lifestyle/2020/04/27/people-across-country-are-delivering-groceries-free-its-solidarity-not-charity/ [accessed 2020-07-25]
- Reger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019-a perfect storm? JAMA Psychiatry 2020 Apr 10:1. [ CrossRef ] [ Medline ]
- Cohn MA, Mehl MR, Pennebaker JW. Linguistic markers of psychological change surrounding September 11, 2001. Psychol Sci 2004 Oct;15(10):687-693. [ CrossRef ] [ Medline ]
- González-Sanguino C, Ausín B, Castellanos MÁ, Saiz J, López-Gómez A, Ugidos C, et al. Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain Behav Immun 2020 Jul;87:172-176 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Labouliere CD, Vasan P, Kramer A, Brown G, Green K, Rahman M, et al. "Zero Suicide" - a model for reducing suicide in United States behavioral healthcare. Suicidologi 2018;23(1):22-30 [ FREE Full text ] [ Medline ]
- Florida R. The lasting normal for the post-pandemic city. Bloomberg. 2020. URL: https://www.bloomberg.com/news/features/2020-06-25/the-new-normal-after-the-coronavirus-pandemic [accessed 2020-07-25]
- Asonye C. There's nothing new about the 'new normal'. Here's why. World Economic Forum. 2020. URL: https://www.weforum.org/agenda/2020/06/theres-nothing-new-about-this-new-normal-heres-why/ [accessed 2020-07-25]
- Rudd BN, Beidas RS. Digital mental health: the answer to the global mental health crisis? JMIR Ment Health 2020 Jun 02;7(6):e18472 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Yoo DW, Birnbaum ML, Van Meter AR, Ali AF, Arenare E, Abowd GD, et al. Designing a clinician-facing tool for using insights from patients' social media activity: iterative co-design approach. JMIR Ment Health 2020 Aug 12;7(8):e16969 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Pendse SR, Lalani FM, De Choudhury M, Sharma A, Kumar N. "Like Shock Absorbers": understanding the human infrastructures of technology-mediated mental health support. In: Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems. 2020 Presented at: CHI '20; April 2020; Honolulu, HI. [ CrossRef ]
- Saha K, Bayraktaroglu AE, Campbell AT, Chawla NV, De Choudhury M, D'Mello SK, et al. Social media as a passive sensor in longitudinal studies of human behavior and wellbeing. In: Extended Abstracts of the 2019 CHI Conference on Human Factors in Computing Systems. 2019 Presented at: CHI '19; May 2019; Glasgow, Scotland. [ CrossRef ]
- Cunha BA. Influenza: historical aspects of epidemics and pandemics. Infect Dis Clin North Am 2004 Mar;18(1):141-155. [ CrossRef ] [ Medline ]
- Aassve A, Alfani G, Gandolfi F, Le Moglie M. Epidemics and trust: the case of the spanish flu. Working Papers 661, Innocenzo Gasparini Institute for Economic Research 2020:1.
- Phillips H. The recent wave of 'Spanish' flu historiography. Social Hist Med 2014 Sep 01;27(4):789-808. [ CrossRef ]
- Huremović D. Psychiatry of Pandemics: a Mental Health Response to Infection Outbreak. Cham, Switzerland: Springer; 2019.
- Ornell F, Schuch JB, Sordi AO, Kessler FHP. "Pandemic fear" and COVID-19: mental health burden and strategies. Braz J Psychiatry 2020;42(3):232-235 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Baumeister RF, Leary MR. The need to belong: desire for interpersonal attachments as a fundamental human motivation. Psychol Bull 1995 May;117(3):497-529. [ Medline ]
- Gao J, Zheng P, Jia Y, Chen H, Mao Y, Chen S, et al. Mental health problems and social media exposure during COVID-19 outbreak. PLoS One 2020;15(4):e0231924 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Best P, Manktelow R, Taylor B. Online communication, social media and adolescent wellbeing: a systematic narrative review. Child Youth Services Rev 2014 Jun;41:27-36. [ CrossRef ]
- Berryman C, Ferguson CJ, Negy C. Social media use and mental health among young adults. Psychiatr Q 2018 Jun;89(2):307-314. [ CrossRef ] [ Medline ]
- Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun 2020 Aug;88:901-907 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Saha K, Torous J, Ernala SK, Rizuto C, Stafford A, De Choudhury M. A computational study of mental health awareness campaigns on social media. Transl Behav Med 2019 Nov 25;9(6):1197-1207 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Nelson BW, Pettitt A, Flannery JE, Allen NB. Rapid assessment of psychological and epidemiological correlates of COVID-19 concern, financial strain, and health-related behavior change in a large online sample. PLoS One 2020;15(11):e0241990 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Lublin N. Notes on coronavirus: how is America feeling? Part 7. Crisis Text Line. 2020. URL: https://www.crisistextline.org/mental-health/notes-on-coronavirus-how-is-america-feeling-part-7/ [accessed 2020-07-25]
- Miltimore J. ‘A Year's Worth of Suicide Attempts in Four Weeks’: the unintended consequences of COVID-19 lockdowns. Foundation for Economic Education. 2020. URL: https://fee.org/articles/a-years-worth-of-suicide-attempts-in-four-weeks-the-unintended-consequences-of-covid-19-lockdowns/ [accessed 2020-07-25]
- Seaman J. Suicides in Colorado dropped 40% during first 2 months of coronavirus pandemic but calls to crisis line spiked. The Denver Post. 2020. URL: https://www.denverpost.com/2020/05/23/colorado-suicides-dropped-coronavirus-pandemic-calls-to-crisis-line-spiked/ [accessed 2020-07-25]
- Jacobson NC, Lekkas D, Price G, Heinz MV, Song M, O'Malley AJ, et al. Flattening the mental health curve: COVID-19 stay-at-home orders are associated with alterations in mental health search behavior in the United States. JMIR Preprints. Preprint posted online on May 26, 2020. [ CrossRef ]
- Mackey T, Purushothaman V, Li J, Shah N, Nali M, Bardier C, et al. Machine learning to detect self-reporting of symptoms, testing access, and recovery associated with COVID-19 on Twitter: retrospective big data infoveillance study. JMIR Public Health Surveill 2020 Jun 08;6(2):e19509 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Stokes DC, Andy A, Guntuku SC, Ungar LH, Merchant RM. Public priorities and concerns regarding COVID-19 in an online discussion forum: longitudinal topic modeling. J Gen Intern Med 2020 Jul;35(7):2244-2247 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Guntuku SC, Sherman G, Stokes DC, Agarwal AK, Seltzer E, Merchant RM, et al. Tracking mental health and symptom mentions on Twitter during COVID-19. J Gen Intern Med 2020 Sep;35(9):2798-2800 [ FREE Full text ] [ CrossRef ] [ Medline ]
- Imran M, Castillo C, Diaz F, Vieweg S. Processing social media messages in mass emergency: survey summary. In: Companion Proceedings of the Web Conference 2018. 2018 Presented at: WWW '18; April 2018; Lyon, France. [ CrossRef ]
- Olteanu A, Castillo C, Diaz F, Kıcıman E. Social data: biases, methodological pitfalls, and ethical boundaries. Front Big Data 2019 Jul 11;2:13. [ CrossRef ]
- Watts DJ. Common sense and sociological explanations. AJS 2014 Sep;120(2):313-351. [ CrossRef ] [ Medline ]
- George Floyd: what happened in the final moments of his life. BBC News. 2020. URL: https://www.bbc.com/news/world-us-canada-52861726 [accessed 2020-07-25]
Abbreviations
Edited by G Eysenbach; submitted 26.07.20; peer-reviewed by B Rudd, B Hoffman; comments to author 11.08.20; revised version received 19.08.20; accepted 26.10.20; published 24.11.20
©Koustuv Saha, John Torous, Eric D Caine, Munmun De Choudhury. Originally published in the Journal of Medical Internet Research (http://www.jmir.org), 24.11.2020.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work, first published in the Journal of Medical Internet Research, is properly cited. The complete bibliographic information, a link to the original publication on http://www.jmir.org/, as well as this copyright and license information must be included.
Experimental Study Designs
Affiliation.
- 1 Department of Anesthesia, Critical Care and Pain Medicine, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA.
- PMID: 33448352
- DOI: 10.1111/head.13928
Publication types
- Biomedical Research* / standards
- Headache Disorders*
- Research Design* / standards

IMAGES
COMMENTS
In the present research, we administered, in two experiments, the imitation-inhibition task - a robust, unobtrusive, and reliable paradigm that is sensitive to self-other focus on a trial-by-trial ...
Browse the 50 most downloaded Nature Communications articles across life and biological sciences published in 2020. ... valuable research from an international community. ... RNA-seq experiments ...
The results of our quasi-experimental study of the effect of implementing a nurse care coordination program in community health centers suggest that adding care coordination to the nursing role is associated with improvement for program enrollees in key program goals, including greater patient access to and engagement with healthcare providers ...
Introduction. The analysis of psychophysiological fatigue is considered very important in different contexts (Lohani et al., 2019).In this sense, the consideration of the study of humans's response to external and internal loads (Wijesuriya et al., 2007; Wilson et al., 2007) has become one of the most important research topics.The external loads exerted on the individual are added to their ...
This study was run on March 12, 2020. We recruited 1,000 participants using Lucid, an online recruiting source that aggregates survey respondents from many respondent providers (Coppock & Mcclellan, 2019). Lucid uses quota sampling to provide a sample that is matched to the U.S. public on age, gender, ethnicity, and geographic region.
Review Article Open Access 18 Dec 2020 Comparison of thrombus, gut, and oral microbiomes in Korean patients with ST-elevation myocardial infarction: a case-control study Ju-Seung Kwun
Recent Updates in Experimental Research and Clinical Evaluation on Drugs for COVID-19 Treatment. Houwen Zou. Houwen Zou. ... 2020). An open-label cohort study assessed the clinical outcome of sarilumab among 28 patients infected by SARS-CoV-2 compared with 28 contemporary patients receiving standard of care alone (Della-Torre et al., 2020). The ...
Conclusions: We studied the psychosocial effects of the COVID-19 crisis by using social media data from 2020, finding that people's mental health symptomatic and support expressions significantly increased during the COVID-19 period as compared to similar data from 2019. ... Large-scale Quasi-Experimental Study on Social Media Psychosocial ...
Experimental Psychology acknowledged the importance of preregistration of study plans and publication of negative study results very early with the introduction of the Registered Report article type. A Registered Report is a preregistered study plan detailing the theoretical background, empirical hypotheses, methods, and data-analytic ...
Experimental Study Designs Headache. 2020 Sep;60(8):1501-1507. doi: 10.1111/head.13928. Author Dana P Turner 1 Affiliation 1 Department of Anesthesia, Critical Care and Pain Medicine, Massachusetts General Hospital, Harvard Medical School, Boston, MA, USA. PMID: 33448352 DOI: 10.1111 ...